MODULE 5: MANAGING TOBACCO CESSATION AND OTHER TOXIC EXPOSURES |
|
Noncommunicable diseases (NCDs) has continually been a main health challenge and tobacco use is an important behavioral risk factors that is responsible for 12% of male deaths and 6% of female deaths worldwide. Tobacco use is the leading cause of preventable death and is estimated to kill more than 5 million people each year worldwide.
According to the WHO, the Philippines is one of the 15 countries worldwide with a heavy burden of tobacco-related health with an estimated smoking prevalence of 33.9% for men, 6.4% for women, 1.34% of boys ages 10-14 and 20.6% of the Philippine’s overall population are daily tobacco smoker. (WHO, Tobacco Free Initiative (TFI), 2015). The tobacco industry here has been described as the “strongest tobacco lobby in Asia” and the Philippines has one of the highest per capita level of cigarette consumption among the ASEAN countries. (B. Bellew, 2013)
The Philippines has made a lot of improvement on tobacco control in the recent years. However, people continue to die and become sick and the cost to health care from tobacco use is still high, killing 117,700 of people of tobacco-caused disease every year. Twenty-two percent more men die in the Philippine than on average in medium-HDI countries. The heavy burden of the disease tobacco use has on the health of our country, we as health professionals have several roles to play in comprehensive tobacco control including role model, clinician, educator, scientist, leader, opinion-builder and alliance builder. All health professionals should at least serve as tobacco-free role models for the general public, address tobacco dependence as part of our standard care of practice, assess exposure to secondhand smoke and provide information about avoiding all exposure. We have a unique role to play in helping tobacco users quit as we can reach as much as 80% of all tobacco users per year. (WHO, Toolkit for delivering the 5A's and 5R's brief tobacco intervention, 2014)
Currently, we do not have a national quitline. A lot of policies and media campaign have been in place to help curb tobacco use. The is a ban on tobacco advertisement on the national TV and radio, local magazines, billboard and outdoor advertising, advertising on internet. In the Philippines 60.61% of the retail price is excise tax. (Atlas, 2020)
According to the WHO, the Philippines is one of the 15 countries worldwide with a heavy burden of tobacco-related health with an estimated smoking prevalence of 33.9% for men, 6.4% for women, 1.34% of boys ages 10-14 and 20.6% of the Philippine’s overall population are daily tobacco smoker. (WHO, Tobacco Free Initiative (TFI), 2015). The tobacco industry here has been described as the “strongest tobacco lobby in Asia” and the Philippines has one of the highest per capita level of cigarette consumption among the ASEAN countries. (B. Bellew, 2013)
The Philippines has made a lot of improvement on tobacco control in the recent years. However, people continue to die and become sick and the cost to health care from tobacco use is still high, killing 117,700 of people of tobacco-caused disease every year. Twenty-two percent more men die in the Philippine than on average in medium-HDI countries. The heavy burden of the disease tobacco use has on the health of our country, we as health professionals have several roles to play in comprehensive tobacco control including role model, clinician, educator, scientist, leader, opinion-builder and alliance builder. All health professionals should at least serve as tobacco-free role models for the general public, address tobacco dependence as part of our standard care of practice, assess exposure to secondhand smoke and provide information about avoiding all exposure. We have a unique role to play in helping tobacco users quit as we can reach as much as 80% of all tobacco users per year. (WHO, Toolkit for delivering the 5A's and 5R's brief tobacco intervention, 2014)
Currently, we do not have a national quitline. A lot of policies and media campaign have been in place to help curb tobacco use. The is a ban on tobacco advertisement on the national TV and radio, local magazines, billboard and outdoor advertising, advertising on internet. In the Philippines 60.61% of the retail price is excise tax. (Atlas, 2020)
health impact
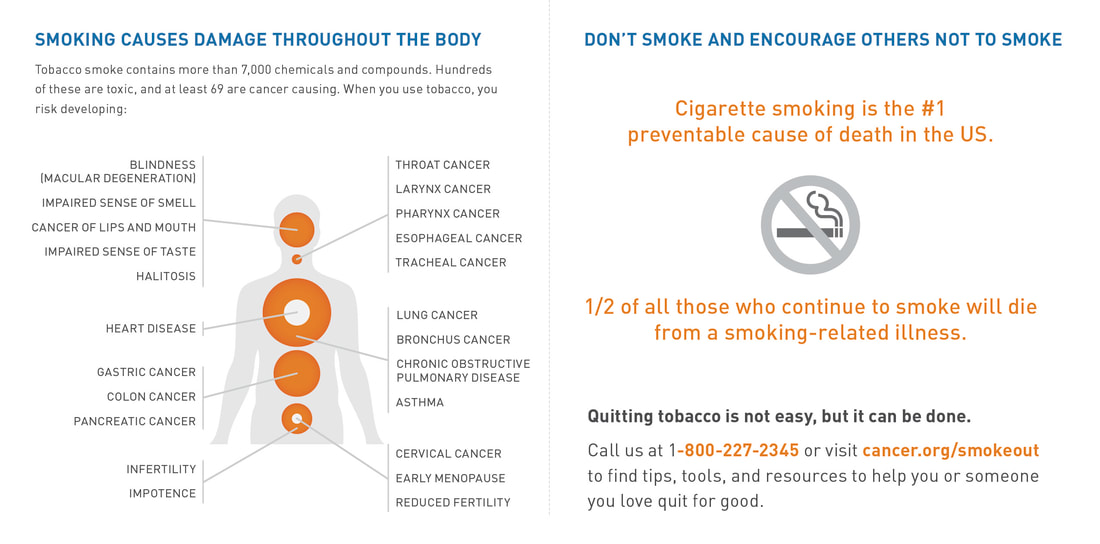
Tobacco products contains more than 7000 chemicals, at least 250 are known to be harmful and at least 69 are known to cause cancer. All tobacco product pose a threat to our health and can damage every part of our body that cause shortness of breath, worsening of asthma and respiratory infections as well as many NCDs including heart disease, stroke, cancer and chronic respiratory diseases that impact the tobacco user and their family. Secondhand smoke exposure increases the risk of having sudden infant death syndrome, acute respiratory illness, middle ear diseases and chronic respiratory symptoms in children, while in adults, it can cause coronary heart disease, nasal irritation, lung cancer and reproductive effects in women causing low birth weight. There has been misconceptions about health risks of smoking most especially in developing countries like the Philippines, who do not completely understand the dangers of tobacco use because of the advertisements these tobacco companies have that distort the real health consequences of smoking.
https://www.usm.edu/sites/default/files/groups/student-health-services-moffitt-health-center/pdf/true-cost-of-smoking-infographic-print.pdf
https://www.usm.edu/sites/default/files/groups/student-health-services-moffitt-health-center/pdf/true-cost-of-smoking-infographic-print.pdf
NICOTINE DEPENDENCE
Smoking can lead to nicotine dependence, the most common form of chemical dependence in the US. Research have shown that nicotine may be as addictive as heroin, cocaine or alcohol and requires repeated treatments. Withdrawal symptoms, stress and weight gain.
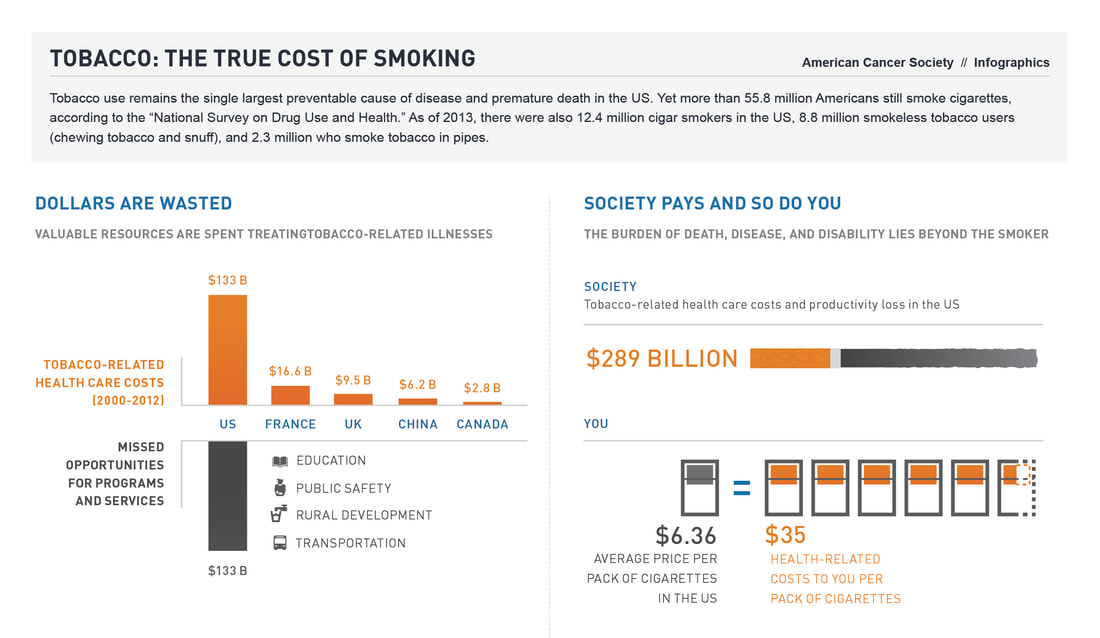
ECONOMIC IMPACT OF TOBACCO USE
Tobacco use is a burden not only due to its health consequences but also on the patient’s economics as well. It is estimated that 5-15% of a smoker’s disposable income is spent on buying cigarettes and more if one suffers from the ill effect tobacco use can bring when it takes a toll on our health. It can cause a lot of suffering for families and individuals associates with smokers and can manifest in the form of diminished quality of life, death and financial burden.
SOCIAL CONSEQUENCES OF TOBACCO USE
Social interactions and relationships have been affected by smoking negatively as it draws people away with the stigma that smokers are smelly, dirty, unhealthy… A lot of people shy away from people who smokes and do not consider having a relationship with smokers. As a smoker, their children are more likely to smoke also and tend to be heavier smokers at a young age.
Smoking can lead to nicotine dependence, the most common form of chemical dependence in the US. Research have shown that nicotine may be as addictive as heroin, cocaine or alcohol and requires repeated treatments. Withdrawal symptoms, stress and weight gain.
ECONOMIC IMPACT OF TOBACCO USE
Tobacco use is a burden not only due to its health consequences but also on the patient’s economics as well. It is estimated that 5-15% of a smoker’s disposable income is spent on buying cigarettes and more if one suffers from the ill effect tobacco use can bring when it takes a toll on our health. It can cause a lot of suffering for families and individuals associates with smokers and can manifest in the form of diminished quality of life, death and financial burden.
SOCIAL CONSEQUENCES OF TOBACCO USE
Social interactions and relationships have been affected by smoking negatively as it draws people away with the stigma that smokers are smelly, dirty, unhealthy… A lot of people shy away from people who smokes and do not consider having a relationship with smokers. As a smoker, their children are more likely to smoke also and tend to be heavier smokers at a young age.
SCREENING NICOTINE DEPENDENCE
Screening of patients for nicotine dependence should be done in each clinic visit. The American Society of Addiction Medicine defines addiction as: (ASAM, 2019) “Addiction is a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences. People with addiction use substances or engage in behaviors that become compulsive and often continue despite harmful consequences. Prevention efforts and treatment approaches for addiction are generally as successful as those for other chronic diseases.”
QUITTING
In the US, 68.0% of adult smokers said that they wanted to quit smoking (CDC, 2015) and 55.1% said that they had made a quit attempt in the past year. (CDC, 2018) However, only 7.5% of those who attempted to quit were successful. Our role as a physician is very important in identifying these patients because only 57.2% of adult smokers who have seen a health professional in the past year reported receiving advice to quit. Even brief advice to quit (<3 minutes) from their healthcare provider improve cessation rates and is highly cost-effective.
HEALTH BENEFITS OF SMOKING CESSATION (WHO, 2020)
Screening of patients for nicotine dependence should be done in each clinic visit. The American Society of Addiction Medicine defines addiction as: (ASAM, 2019) “Addiction is a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences. People with addiction use substances or engage in behaviors that become compulsive and often continue despite harmful consequences. Prevention efforts and treatment approaches for addiction are generally as successful as those for other chronic diseases.”
QUITTING
In the US, 68.0% of adult smokers said that they wanted to quit smoking (CDC, 2015) and 55.1% said that they had made a quit attempt in the past year. (CDC, 2018) However, only 7.5% of those who attempted to quit were successful. Our role as a physician is very important in identifying these patients because only 57.2% of adult smokers who have seen a health professional in the past year reported receiving advice to quit. Even brief advice to quit (<3 minutes) from their healthcare provider improve cessation rates and is highly cost-effective.
HEALTH BENEFITS OF SMOKING CESSATION (WHO, 2020)
- Within 20 mins, heart rate and blood pressure drop
- In 12 hours, the carbon monoxide level in your blood drops to normal
- 1-9 months, coughing decreases and shortness of breath improves
- 1 year, coronary heart disease risk decreases by half compared to smokers
- 5-15 years after quitting, stroke risk is reduced to that of a non smoker
- 10 years, lung cancer risk is halved and cancer of the mouth, throat, esophagus, bladder, cervix, and pancreas risk decreases.
- 15 years, coronary heart disease risk is same with non smokers.
ECONOMIC BENEFITS OF SMOKING CESSATION (WHO, 2020)
- Quitting has a very clear and tangible financial benefits for smokers.
SOCIAL BENEFITS OF SMOKING CESSATION (WHO, 2014)
- After quitting, patients will feel less isolated - quitting means they can go anywhere, not just where they can smoke. They will improve their relationships with their family, friends and employers. They will be more productive - they don’t have to keep stopping what they are doing to have a smoke. They will be able to expand their social interactions. When patients quit smoking, their children become less likely to start smoking and more likely to quit if they already smoke.”
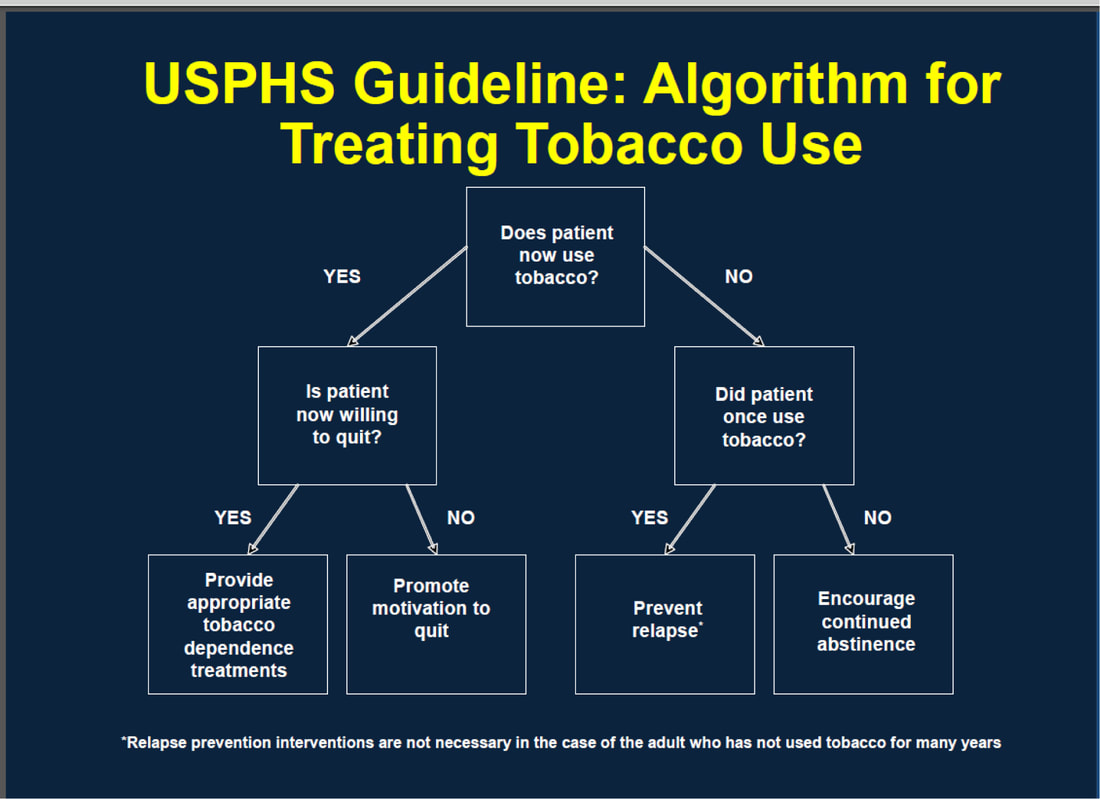
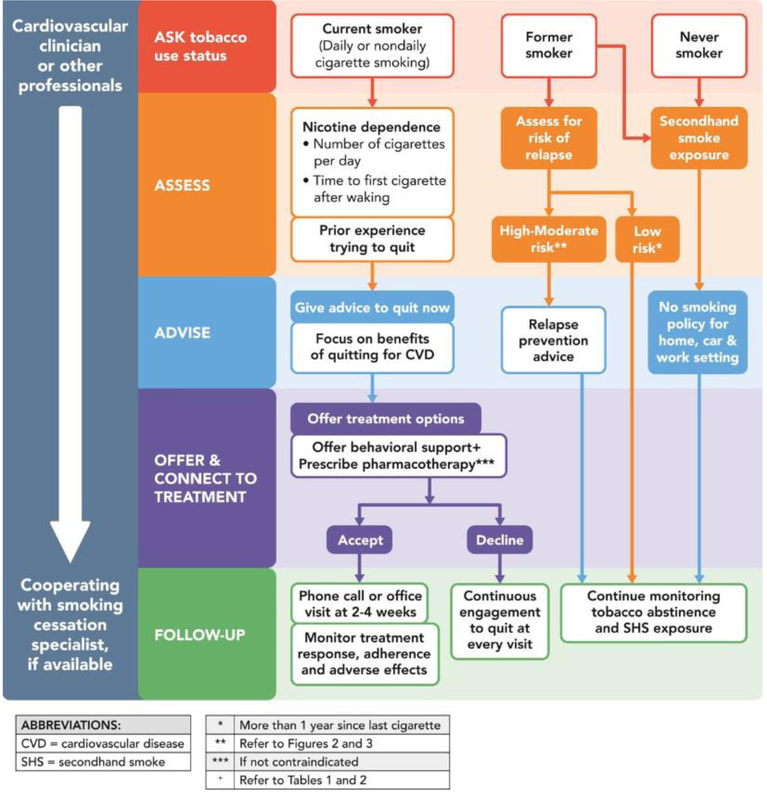
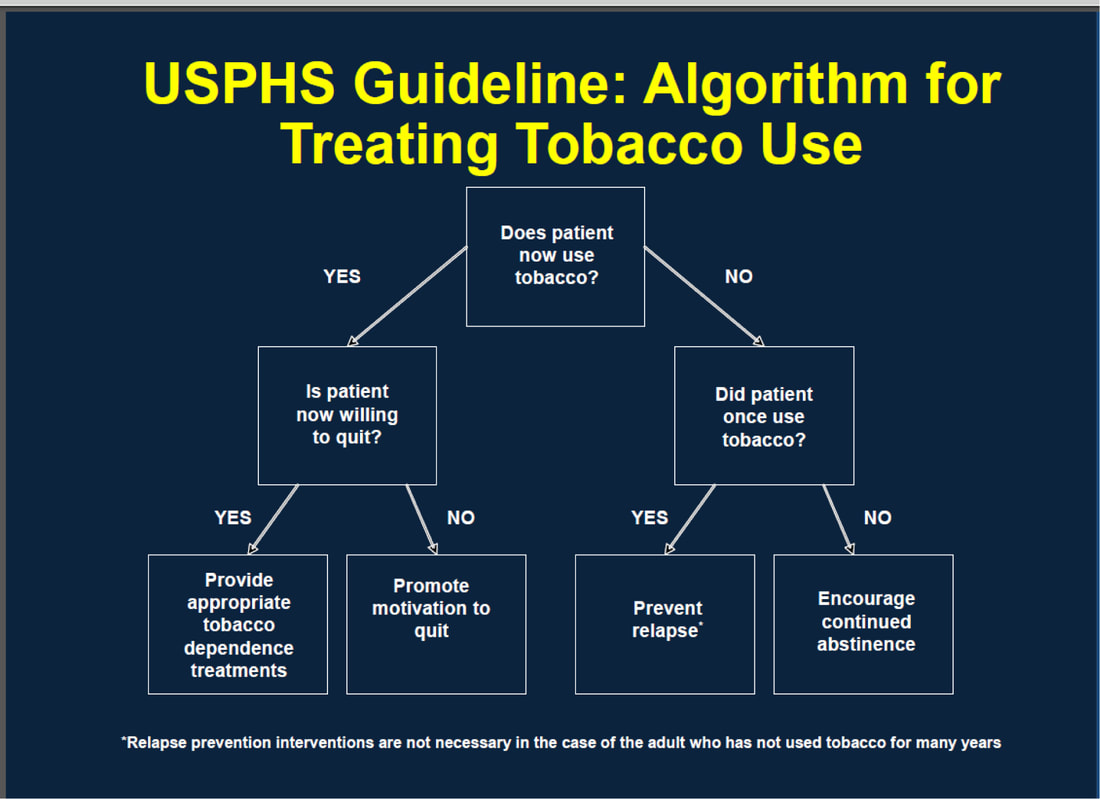
TOBACCO CESSATION
Counseling and medication are both effective for treating tobacco dependence, and using them together is more effective than using either alone. Create effective, evidence-based tobacco cessation treatment plans using the USPHS Tobacco Cessation Guideline, 5As model with brief interventions.
SCREENING TOOL FOR NICOTINE DEPENDENCE: FAGERTROM TEST
https://ndri.curtin.edu.au/btitp/documents/Fagerstrom_test.pdf
TREATMENT FOR SMOKERS WHO WANT TO QUIT
Both the providers and tobacco users must be persistent when it comes to quitting, and most cases, repeated intervention is necessary. Lapses and relapses are common and although 70% of tobacco users want to quit, only 5% succeed without assistance. Most tobacco users try to quit on their own, but more than 95% relapse. Physicians using evidence-based programs can more than double successful quit rates.
US PUBLIC HEALTH SERVICE CLINICAL PRACTICE GUIDELINE
The USPHS offers providers guidance on evidence-based treatments, their effectiveness, and systems changes that can increase tobacco assessment, intervention and cessation rates among patients. USPHS includes 10 key recommendations:
SCREENING TOOL FOR NICOTINE DEPENDENCE: FAGERTROM TEST
https://ndri.curtin.edu.au/btitp/documents/Fagerstrom_test.pdf
TREATMENT FOR SMOKERS WHO WANT TO QUIT
- Brief intervention
- Individual, group or telephone counseling
- Behavioral therapies (enhancing problem solving skills)
- Treatment with more person-to-person contact and intensity
- Programs to deliver treatments using mobile phones
- Medications (OTC/Rx nicotine replacement therapy + Rx non-nicotine medications)
Both the providers and tobacco users must be persistent when it comes to quitting, and most cases, repeated intervention is necessary. Lapses and relapses are common and although 70% of tobacco users want to quit, only 5% succeed without assistance. Most tobacco users try to quit on their own, but more than 95% relapse. Physicians using evidence-based programs can more than double successful quit rates.
US PUBLIC HEALTH SERVICE CLINICAL PRACTICE GUIDELINE
The USPHS offers providers guidance on evidence-based treatments, their effectiveness, and systems changes that can increase tobacco assessment, intervention and cessation rates among patients. USPHS includes 10 key recommendations:
- Tobacco dependence is a chronic disease that requires repeated intervention and multiple attempts to quit. Effective treatments exist that can significantly increase rates of long-term abstinence.
- It is important that physicians can identify and tobacco use status and treat every tobacco user seen in healthcare setting.
- Tobacco dependence treatments are effective ang physicians should encourage every patient willing to make a quit attempt to use the counseling treatments and medications recommended.
- Brief tobacco dependence treatment is effective. Every physician should offer every patient who uses tobacco at least the brief treatments shown to be effective in this guideline
- Individual, group and telephone counseling are effective and their effectiveness increases with treatment intensity. Practical counseling (problem solving/skills training) and social support delivered as part of treatment.
- There are numerous effective medications for tobacco dependence and clinicians should encourage their use by all patients who wants to quit smoking, except for pregnant women, smokeless tobacco uses, light smokers and adolescents wherein there is insufficient evidence of effectiveness. Physicians should also consider the use of certain combinations of medications identified as effective in USPHS Guideline.
- Counseling and medications are effective when used alone for treating tobacco dependence, however, combination of counseling and medication is more effective than either alone.
- Telephone quitline counseling is effective that can reach diverse populations and has a broader reach, thus patient should have access to quitlines and promote quitline use.
- If ever a tobacco user is unwilling to make a quit attempt, motivation treatments should be used to effectively increase future quit attempts.
- Tobacco dependence treatments are both clinically effective and highly cost-effective relative to interventions for other clinical disorders.
The 5A’s model is used to all tobacco users despite their willingness and motivation to quit. Patients are assessed for their willingness to quit, then assisted by providing evidence-based treatment. If the patient is not yet willing to quit, we increase their motivation to increase their readiness for change. Those who have recently quit or are facing ongoing challenges are provided relapse prevention. Follow-up plans are provided for all of them. If there is time constraints, we ask every patient about their tobacco use every time they visit us and Advise tobacco users to quit and refer tobacco users for behavioral support and intensive treatment.
FACILITATING BEHAVIORAL CHANGE WITH PATIENTS WHO ARE WILLING TO QUIT
ASK- Identify all tobacco users at every visit
ADVISE-strongly urge all tobacco users to quit
ASSESS- determine willingness to make a quit attempt
-Patient is willing to make a quit attempt, provide assistance
-Patient will participate in an intensive treatment, deliver or refer to an intensive intervention
-Patient is unwilling to make a quit attempt, provide motivational intervention to increase future quit attempts
ASSIST- Help the patient quit by providing counseling and medication.
- Set a quit date (ideally within 2 weeks)
- Involve family and friends about quitting and ask for support
- Anticipate challenges especially during the first two weeks including nicotine withdrawal symptoms.
- Remove tobacco products from sight (e.g. home, car, work, etc.)
-Abstinence (strive for total abstinence after the quit date)
-Past quit experiences (challenges, and near success stories, etc…)
-Anticipated challenges and triggers in upcoming attempt
-Alcohol and other triggers
-Other smokers in the household
-local quit lines
ARRANGE: Ensure follow-up contact
-Follow-up should begin soon after the quit date, preferably during the 1st week
-Second follow-up is recommended within the first month
- then schedule follow-up as indicated
Implementation Strategies 2:
-Identify problems encountered and anticipate upcoming challenges
-Assess medication use and problems
-Remind patients of quit-line support
-Address tobacco use at next clinical visit
-If patient has quit, acknowledge their efforts and congratulate on their success
ASK- Identify all tobacco users at every visit
- Action: Ensure to ask all patients every clinic visit on tobacco use and document them.
- Implementation Strategies: include tobacco use as a necessary vital sign in every clinic visit.
ADVISE-strongly urge all tobacco users to quit
- Action: Urge all tobacco users to quit in a clear, strong and personalized manner
- Implementation Strategies: advise should be clear (occasional smoking or light smoking is still dangerous), strong (quitting smoking is the most important thing that you can do to protect your health), personalized (continuing to smoke makes your asthma worse and quitting may dramatically improve your health).
ASSESS- determine willingness to make a quit attempt
- Action: assess every tobacco user’s willingness to make a quit attempt at this time.
-Patient is willing to make a quit attempt, provide assistance
-Patient will participate in an intensive treatment, deliver or refer to an intensive intervention
-Patient is unwilling to make a quit attempt, provide motivational intervention to increase future quit attempts
ASSIST- Help the patient quit by providing counseling and medication.
- Action: assist patient with a quit plan
- Set a quit date (ideally within 2 weeks)
- Involve family and friends about quitting and ask for support
- Anticipate challenges especially during the first two weeks including nicotine withdrawal symptoms.
- Remove tobacco products from sight (e.g. home, car, work, etc.)
- Action: recommend approved medications except when contraindicated or in certain populations where there is insufficient evidence for its effectiveness (e.g. pregnant women, smokeless tobacco users, light smokers and adolescents)
- Action: provide practical counseling (problem-solving/skills training)
-Abstinence (strive for total abstinence after the quit date)
-Past quit experiences (challenges, and near success stories, etc…)
-Anticipated challenges and triggers in upcoming attempt
-Alcohol and other triggers
-Other smokers in the household
- Action: Provide intra-treatment social support
- Action: provide supplementary materials, including information on ( or referrals to) quit lines
-local quit lines
ARRANGE: Ensure follow-up contact
- Action: arrange follow-up either in person, via telephone or online
-Follow-up should begin soon after the quit date, preferably during the 1st week
-Second follow-up is recommended within the first month
- then schedule follow-up as indicated
Implementation Strategies 2:
-Identify problems encountered and anticipate upcoming challenges
-Assess medication use and problems
-Remind patients of quit-line support
-Address tobacco use at next clinical visit
-If patient has quit, acknowledge their efforts and congratulate on their success
STAGE OF CHANGE FOR SMOKING CESSATION
- Precontemplation: current smokers who are not planning on quitting smoking in the next 6 months
- Contemplation: Current smokers who are planning on quitting smoking in the next 6 months but have not made a quit attempt in the past year.
- Preparation: current smokers who are definitely planning to quit within next 30 days and have made a quit attempt in the past year
- Action: individual who are not currently smoking and have stopped smoking within the past 6 months.
- Maintenance: individuals who are not currently smoking and have stopped smoking for longer than 6 months but less than 5 years
POINTS TO CONSIDER
- 3-minute minimal intervention increases the overall tobacco abstinence rates. Every tobacco user should be offered at least minimal intervention, whether or not he or she is referred to an intensive intervention.
- Intensive interventions are more effective than less intensive interventions shown in a dose-response relation between session length of person-to-person contact and successful treatment outcomes.
- Four or more sessions of person-to-person treatment delivery is effective in increasing abstinence rates. We should strive to meet the patients at least four or more times in those quitting tobacco use.
- Proactive telephone counseling, group counseling and individual counseling formats are effective
- Smoking cessation interventions that are delivered in multiple formats increase abstinence rates and should be encouraged.
- Tailored materials, print and web-based, appear to be effective in helping people quit.
- Counseling and behavior therapies result in higher abstinence rate
- Provide support and encouragement as part of treatment (encourage patient to talk about the process one is undergoing while quitting, challenges, barriers, triggers, etc.)
- Other treatment modalities that do not show evidence of effectiveness
- Acupuncture, Hypnosis
- Physiological feedback, restricted environmental stimulation therapy, use of incentives, and cigarette fading
Electronic nicotine delivery systems like e-cigarettes, e-hookah are not FDA-regulated devices and are not FDA-approved as tobacco cessation treatments.
Additional readings:
Toolkit for delivering the 5A's and 5R's brief tobacco interventions in primary care
Additional readings:
Toolkit for delivering the 5A's and 5R's brief tobacco interventions in primary care
BEHAVIOR THERAPY WITH PHARMACOTHERAPY
Nicotine not only cause pathophysiological changes in the smoker’s body but one can also develop tolerance to its own action with repeated use. Repeated nicotine exposure develops neuroadaptation of the receptors resulting in tolerance. Lifestyle medicine approach emphasizes non-pharmacological therapies for smoking cessation. Pharmacological therapies are used as a supplement to the lifestyle approach, as needed. Pharmacotherapies for smoking cessation should reduce withdrawal symptoms and block the reinforcing effects of nicotine without causing excessive adverse effects.
The ritual involved in tobacco use, from opening a pack of cigarette to lighting it and the sight and smell of smoke is one of the strangest of human behavior. Why should one do such act that could not prolong one’s life but instead acknowledged by the smoker’s themselves that it could lead to death and devastation, and is distasteful even?
Nicotine is the primary chemical in tobacco use that can activate the brain-reward system by increasing dopamine release as it is a potent pyscho-active drug. This brain reward system is a common pathway for pleasurable activities in most drugs of addiction. The euphoria one feels act as a reinforcer for its continued use. This peak in plasma nicotine level and the transient activation of the reward system is followed by a gradual fall in nicotine levels into a state of withdrawal, which is again relieved by the next cigarette. Dependence arise from the temporary rituals and sensory inputs with the repeated stimulation and relief of withdrawal symptoms. This explains why nicotine replacement therapy products, that deliver nicotine slowly and do not produce high plasma nicotine levels, have minimal addictive potential. (Jiloha, 2014)
The ritual involved in tobacco use, from opening a pack of cigarette to lighting it and the sight and smell of smoke is one of the strangest of human behavior. Why should one do such act that could not prolong one’s life but instead acknowledged by the smoker’s themselves that it could lead to death and devastation, and is distasteful even?
Nicotine is the primary chemical in tobacco use that can activate the brain-reward system by increasing dopamine release as it is a potent pyscho-active drug. This brain reward system is a common pathway for pleasurable activities in most drugs of addiction. The euphoria one feels act as a reinforcer for its continued use. This peak in plasma nicotine level and the transient activation of the reward system is followed by a gradual fall in nicotine levels into a state of withdrawal, which is again relieved by the next cigarette. Dependence arise from the temporary rituals and sensory inputs with the repeated stimulation and relief of withdrawal symptoms. This explains why nicotine replacement therapy products, that deliver nicotine slowly and do not produce high plasma nicotine levels, have minimal addictive potential. (Jiloha, 2014)
USPHS RECOMMENDATION
Clinicians should encourage all patients attempting to quit to use effective medications for tobacco dependence treatment except where contraindicated or for specific populations for which there is insufficient evidence of effectiveness like pregnant women, smokeless tobacco users, light smokers and adolescents.
All forms of nicotine replacement therapy (NRT)-gum, patches and inhalers, -and bupropion are safe and effective for increasing smoking cessation rates in the short and long-term use. Combination NRT may be indicated in patients who have failed monotherapy.
Clinicians should encourage all patients attempting to quit to use effective medications for tobacco dependence treatment except where contraindicated or for specific populations for which there is insufficient evidence of effectiveness like pregnant women, smokeless tobacco users, light smokers and adolescents.
All forms of nicotine replacement therapy (NRT)-gum, patches and inhalers, -and bupropion are safe and effective for increasing smoking cessation rates in the short and long-term use. Combination NRT may be indicated in patients who have failed monotherapy.
FIRST-LINE MEDICATIONS FOR TOBACCO CESSATION
Nicotine replacement therapies (NRT) (5)
The general principle of replacement therapies is to present the patients with a safer and more therapeutically manageable form of the drug that directly alleviates the signs and symptoms of withdrawal and cravings. It uses products that supply low doses of nicotine. The goal of therapy is to cut down on cravings for nicotine and ease the symptoms of nicotine withdrawal.
TYPES OF NICOTINE REPLACEMENT THERAPY
Nicotine supplements come in many forms:
1. Nicotine patch
All nicotine patches are placed and used in similar ways:
Follow the instructions that comes with the package.
The spray gives a quick dose of nicotine to satisfy a craving you are unable to ignore. Levels of nicotine peak within 5 to 10 minutes after using the spray.
Non-nicotine medications (Rx only)
Second-line medications for tobacco cessation (off labels, not FDA-approved for tobacco cessation)
Nicotine replacement therapies (NRT) (5)
The general principle of replacement therapies is to present the patients with a safer and more therapeutically manageable form of the drug that directly alleviates the signs and symptoms of withdrawal and cravings. It uses products that supply low doses of nicotine. The goal of therapy is to cut down on cravings for nicotine and ease the symptoms of nicotine withdrawal.
TYPES OF NICOTINE REPLACEMENT THERAPY
Nicotine supplements come in many forms:
- Gum
- Inhalers
- Lozenges
- Nasal spray
- Skin patch
1. Nicotine patch
All nicotine patches are placed and used in similar ways:
- A single patch is worn each day. It is replaced after 24 hours.
- Place the patch on different areas above the waist and below the neck each day.
- Put the patch on a hairless spot.
- People who wear the patches for 24 hours will have fewer withdrawal symptoms.
- If wearing the patch at night causes odd dreams, try sleeping without the patch.
- People who smoke fewer than 10 cigarettes per day or who weigh less than 99 pounds (45 kilograms) should start with a lower dose patch (for example, 14 mg).
Follow the instructions that comes with the package.
- If your patient is just starting to quit, let them chew 1 to 2 pieces each hour. DO NOT chew more than 20 pieces a day.
- The gum is chewed slowly until it develops a peppery taste. Then, keep it between the gum and cheek and store it there. This lets the nicotine be absorbed.
- Wait at least 15 minutes after drinking coffee, tea, soft drinks, and acidic beverages before chewing a piece of gum.
- People who smoke 25 or more cigarettes per day have better results with the 4 mg dose than with the 2 mg dose.
- The goal is to stop using the gum by 12 weeks.
- The nicotine inhaler looks like a plastic cigarette holder.
- Insert nicotine cartridges into the inhaler and "puff" for about 20 minutes. Do this up to 16 times a day.
- The inhaler is quick-acting. It takes about the same time as the gum to act. It is faster than the 2 to 4 hours it takes for the patch to work.
- The inhaler satisfies oral urges.
- Most of the nicotine vapor does not go into the airways of the lung. Some people have mouth or throat irritation and cough with the inhaler.
- It can help to use the inhaler and patch together when quitting.
The spray gives a quick dose of nicotine to satisfy a craving you are unable to ignore. Levels of nicotine peak within 5 to 10 minutes after using the spray.
- Follow your provider's instructions about how to use the spray. When your patient is starting to quit, you may tell them to spray 1 to 2 times in each nostril, every hour and not spray more than 80 times in 1 day.
- The spray should not be used for longer than 6 months.
- The spray can irritate the nose, eyes, and throat. These side effects often go away in a few days.
Non-nicotine medications (Rx only)
- Varenicline (Chantix) 0.5mg to 1mg; 0.5mg once a day for 1-3 days, 0.5mg twice a day for 4-7 days, 1mg twice a day from day 8 to the end of the treatment which is for a duration of 12 weeks.
- Bupropion SR (Zyban) 150mg per day for 3 days, then 150mg twice a day for 7-12 weeks(smoking quit date 1-2 weeks after beginning medication)
Second-line medications for tobacco cessation (off labels, not FDA-approved for tobacco cessation)
- Clonidine (Rx only) 0.15-0.75mg/day
- Nortriptyline (Rx only)
- Use should be on a case to case basis after first-line medications has been used without success or are contraindicated.
PHARMACOLOGY GUIDELINES
- Familiarity with medication use
- Contraindications
- Patient preference
- Previous patient experience
- Clinical profile of patients like, history of depression, concerns about weight gain, etc.
- Frequency of tobacco use/level of dependence
- Pharmacotherapy for light smokers (<10 cigarettes/day) has no demonstrated benefits
PHARMACOLOGICAL CONSIDERATIONS
Weight gain
- Bupropion SR and nicotine replacement therapies (gum and 4mg lozenges) may delay but not prevent weight gain
- Average weigh gain from tobacco cessation is less than 10 pounds and is more common among women.
Patients with mental illness
- Need higher doses, longer treatment duration and need combination of medications
- Patients with bipolar disorder should not receive bupropion, patch is suggested
- Patch is effective for those with schizophrenia
- Quitting can increase the effect of some psychiatric medication, thus dose adjustments may be needed.
- Check mental illness relapse with changes in smoking status
Patients with CVD history
- No association between nicotine patch and acute cardiovascular events, even in patient who continue to smoke while on the patch
- NRT packaging recommends caution in patients with acute cardiovascular disease
Pregnant smokers
- Counseling is the best choice
- Premature birth or stillbirth caused by smoking may be higher than birth defects caused by NRT use
- Buproprion SR and Varenicline are both category C
- Prescription NRT is category D
Adolescents
- NRT shown to be safe
- Very little evidence to support that medications are helpful in this population and is not a recommended intervention
Long term pharmacotherapy is helpful for tobacco users with persistent withdrawal symptoms and NRT does not present a known health risk when used for long term. Bupropion SR can be used for up to 6 months and Varenicline is recommended for 12 weeks and may repeat for 12 weeks more.
Combining medications
- Patch + gum or nasal spray increases long-term abstinence
- Patch + inhaler is effective
- Patch + bupropion is more effective than patch along
- Patch + nortriptyline increases long-term abstinence
- Combining varenicline + NRT is not recommended
FACILITATING BEHAVIOR CHANGE
Motivational Interviewing can increase the likelihood of future quit attempts. We use relevance, risks, rewards, roadblocks and repetition.
Principles of motivational interviewing:
Express empathy
Reflect words or meaning
Summarize
Normalize feelings and concerns
Support the patient’s autonomy and right to choose or reject change
Develop discrepancy
Reinforce and support “change talk” and “commitment” language
Build and deepen commitment to change
Roll with resistance
Ask permission to provide information
Support self-efficacy
Motivational Interviewing can increase the likelihood of future quit attempts. We use relevance, risks, rewards, roadblocks and repetition.
Principles of motivational interviewing:
Express empathy
- Use open ended questions to explore the importance of addressing smoking or other tobacco use. (How important do you think it is for you to quit smoking?)
- Use open ended questions to explore concerns and benefits of quitting. ( What might happen if you quit?)
- Use reflective listening to seek shared understanding
Reflect words or meaning
- “So you think smoking helps you relieve your stress.”
Summarize
- For example: “what you are telling me is that smoking helps relieve your stress, on the other hand, your wife hates your smoking and you are worried about your children’s health)
Normalize feelings and concerns
- “A lot of people worry about managing their stress without cigarettes.”
Support the patient’s autonomy and right to choose or reject change
- It seems you are not ready to quit smoking right now. Just know that when you are ready, I am here to help you.
Develop discrepancy
- Point out the discrepancy between your patient’s present behavior and expressed priorities, values and goals.– “It seems that you value your family’s health. How do you think your smoking is affecting your children?”
Reinforce and support “change talk” and “commitment” language
- “You notice how smoking is affecting your day to day activities, it has affected your breathing and your work.”
- “It is good that you are thinking of quitting smoking when you get through this important project that you are doing.”
Build and deepen commitment to change
- “there are effective treatments that will help you in the quitting process, including counseling and medication use.”
- “We are here to help you avoid a cardiac events like your brother had last month.”
Roll with resistance
- Be sensitive to your patient’s feelings and back off and use reflection when the patient expresses resistance. “Seems like you are pressured about quitting smoking."
- Express empathy. “You are concerned about gaining weight if you quit smoking.”
Ask permission to provide information
- Would you want me to share with you effective strategies that can help you quit smoking?”
Support self-efficacy
- Listen to patient’s past successes and build on that. Acknowledge them. “You were able to quit smoking for month, I know it was very challenging but you managed to do that for a month.”
- Offer options for achievable small steps toward change.
- Change smoking patterns like no smoking while in the car
- Ask the patient to share quitting strategies that he might find him able to do
FACILITATING BEHAVIOR CHANGE (5Rs)
This is designed to motivate smokers who are unwilling to quit at this time. Smokers may have misinformation, may have concern about the effects of quitting or lack self-confidence because of previous unsuccessful quit attempt
Relevance:
- – Help patient identify why quitting is personally relevant to them. Be specific.
- – If the patient can identify the importance and relevance of quitting smoking to his goals and values in life, he or she is more likely to be motivated to quit tobacco use.
Risk:
- – physicians should ask the patient to identify the harmful effects of smoking and its consequences -health, economic and social and highlight those that is relevant to the patient
- -examples: shortness of breath, worsening of asthma attacks, harm to baby during pregnancy, impotence and infertility, heart attack and strokes, cancers, COPDs, osteoporosis, long term disability, increase risk of lung cancer and heart disease in spouse and increase respiratory illnesses among children, increased risk for low birth weight, middle ear disease, sudden infant death syndrome.
Rewards:
- Ask the patient to state possible benefits of stopping tobacco use and highlight them when they are relevant to the patient and includes:
- Economic: savings gained from not buying a cigarette, money saved because of less hospitalizations not only of oneself but also children and spouse.
- Health: improved health, wellness and quality of life, improved sense of smell and taste, feel better about yourself, healthier kids, improved appearance including reduced wrinkling/aging of skin and whiter teeth
- Social/Environment: home, car, clothing, breath will smell better, you can socialize more with friends without having to worry of cigarette breath and smoke exposure of friends, kids and family members to the effects of tobacco use. Setting a good example for children and decreasing the likelihood that they will smoke.
Roadblocks:
- Barriers or obstacles to quitting should be identified and discuss potential solutions (problem solving counseling, medication) that address these barriers.
- Withdrawal symptoms, fear of failure, weight gain, lack of support, depression, enjoyment of tobacco, being around other tobacco users, limited knowledge of effective treatment options.
Repetition:
- Motivational intervention should be repeated every time to an unmotivated patient every clinic visit.
- Patients who failed in previous attempts should be informed that most patients make repeated quit attempts before they eventually succeed, and that you are there to support them and help them when they fail again.
There is a strong correlation between the number of counseling session combined with medication and the likelihood of successful smoking cessation. Thus, physicians should provide multiple counseling sessions, in addition to medication, to patients who are trying to quit smoking. (Strength of evidence=A).
DIAGNOSTIC CRITERIA FOR SUBSTANCE USE DISORDERS
- Cravings and urges to use the substance
- wanting to cut down or stop but not managing to
- taking the substance in larger amounts or for loner than one is meant to
- neglecting other parts of one’s life because of the substance use
- continuing to use, even when it causes problems in relationships
- using substances even when it puts you in danger.
- Spending a lot of time getting, using, or recovering from substance use.
- Not managing to do what you should at home, work, or school because of substance use
- Giving up important social, occupational, or recreational activities because of substance use.
- Needing more of the substance to get the effect you want (tolerance)
- Development of withdrawal symptoms, which can be relieved by taking more of the substance
SEVERITY OF SUBSTANCE ABUSE USE
- Mild substance use disorder: 2-3 symptoms
- Moderate substance use disorder: 4-5 symptoms
- Severe substance use disorder: 6 or more symptoms
The DSM-5 recognizes substance-related disorders resulting from the use of 10 separate classes of drugs: alcohol; caffeine; cannabis; hallucinogens (phencyclidine or similarly acting arylcyclohexylamines, and other hallucinogens, such as LSD); inhalants; opoids, sedatives, hypnotics or anxiolytics; stimulants (including amphetamine-type substances, cocaine and other stimulants); tobacco and other or unknown substances. Activation of the brain’s reward system is central to problems arising from drug use.
Because of the rewarding feeling people experience as a result of taking the drugs, one may neglect other normal activities in favor of taking the drug. Although the mechanism of action are different for each type of substances prone to abuse, it is the activation of the reward system which is similar across substances, that produces feelings of pleasure or euphoria that make one to use the substances.
SCREENING TOOLS FOR SUBSTANCE USE AND RELATED HEALTH EFFECTS
We as healthcare providers should be able to screen all patients on substance use, as screening may only take 1 minute to do. If we are not able to screen patients for these substance use and abuse, we are will not be able to help our patients.
OTHER CONSIDERATIONS
- Discuss indications for referral to a substance use disorder specialist
- Create effective, evidence-based substance use disorder treatment plans using the 5As model and brief interventions.
ARTICLE REVIEW
- Role of exercise in the treatment of alcohol use disorders
- TAPS tools for primary care patients
- 2018 ACC Expert Consensus Decision Pathway on Tobacco Cessation Treatment
ADDITIONAL RESOURCES
VIDEO REVIEW
- Can alcohol cause cancer
assessment tools
TASKS |
Reflective Journal
|
Deadline for completion: October 9, 2022