EMOTIONAL AND MENTAL HEALTH - MODULE 2 |
acute stress responses
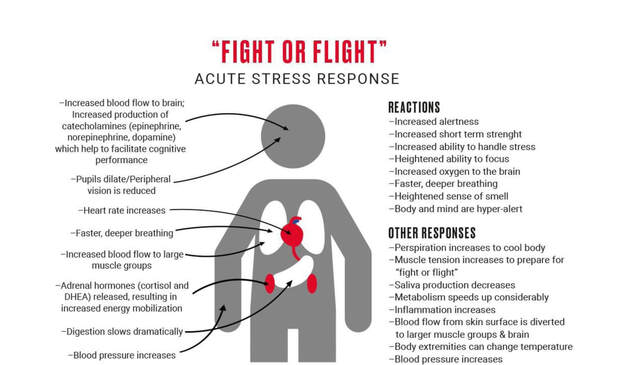
Following the perception of an acute stressful event, there is a cascade of changes in the nervous, cardiovascular, endocrine, and immune systems. These changes constitute the stress response and are generally adaptive, at least in the short term.
The following occur in response to acute stress:
The following occur in response to acute stress:
- Stress hormones are released to make energy stores available for the body’s immediate use.
- Energy is diverted to the tissues that become more active during stress, primarily the skeletal muscles and the brain.
- Cells of the immune system are also activated and migrate to “battle stations”.
- Less critical activities are suspended, such as digestion and the production of growth and gonadal hormones.
- During times of acute crisis, physical integrity and survival are prioritized over eating, growth, and sexual activity.
- Stress hormones are produced by the SNS and hypothalamic-pituitary adrenocortical axis.
- The SNS stimulates the adrenal medulla to produce catecholamines (e.g., epinephrine).
- The paraventricular nucleus of the hypothalamus produces corticotropin releasing factor (CRH) à pituitary gland stimulated to produce adrenocorticotropin à adrenal cortex stimulated to secrete cortisol
- Together, catecholamines and cortisol increase available sources of energy by promoting lipolysis and the conversion of glycogen into glucose.
- Energy is then distributed to the organs that need it most by increasing blood pressure levels
- Increase HR & stroke volume = increase cardiac output
- Contracting certain blood vessels while dilating others
- Activation of the immune system
- Cells of the innate immune system (e.g., macrophages and natural killer cells), the first line of defense, depart from lymphatic tissue and spleen and enter the bloodstream, temporarily raising the number of immune cells in the circulation (i.e., leukocytosis).
- From there, the immune cells migrate into tissues that are most likely to suffer damage during physical confrontation. Once at “battle stations,” these cells are in position to contain microbes that may enter the body through wounds and thereby facilitate healing.
chronic stress response
The acute stress response can become maladaptive if it is repeatedly or continuously activated.
Chronic SNS stimulation of the cardiovascular system due to stress leads to sustained increases in blood pressure and vascular hypertrophy.
Chronic SNS stimulation of the cardiovascular system due to stress leads to sustained increases in blood pressure and vascular hypertrophy.
- The muscles that constrict the vasculature thicken, producing elevated resting blood pressure, and/or it gains a tendency to respond to all types of stressors with a vascular response.
- Leads to hypertrophy of the left ventricle
- Chronically elevated and rapidly shifting BP can lead to damaged arteries and plaque formation
- Th1 and Th2 cytokines become dysregulated and lead both to suppressed humoral and cellular immunity.
- Th1 cytokines mediate cellular immunity by stimulating natural killer cells and cytotoxic T cells, immune cells that target intracellular pathogens (e.g., viruses).
- Th2 cytokines mediate humoral immunity by stimulating B cells to produce antibody, which “tags” extracellular pathogens (e.g., bacteria) for removal.
- Leads to slower wound healing and recovery, poorer antibody responses, and increased vulnerability to viral infections.
stress and the brain
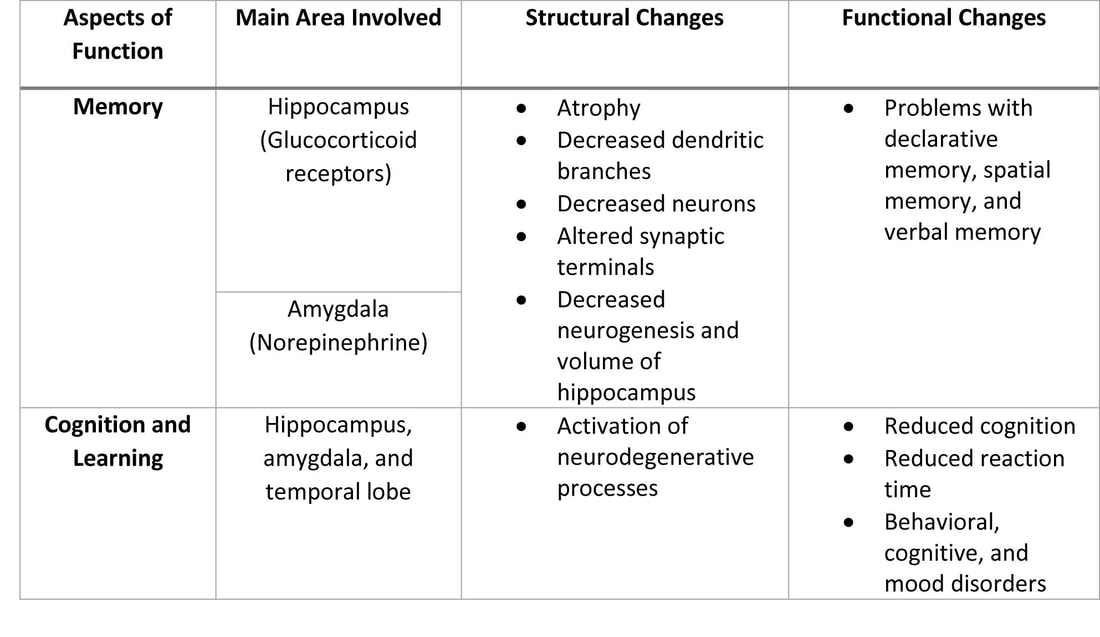
The effects of stress on the nervous system have been investigated for 50 years. Some studies have shown that stress has many effects on the human nervous system and can cause structural changes in different parts of the brain. Chronic stress can lead to atrophy of the brain mass. This can cause changes in the response to stress, cognition and memory.
Memory is one of the important functional aspects of the CNS. Short term memory is dependent on the function of the frontal and parietal lobes, while long-term memory depends on the function of large areas of the brain. However, total function of memory and the conversion of short-term memory to long-term memory are dependent on the hippocampus; an area of the brain that has the highest density of glucocorticosteroid receptors and also represents the highest level of response to stress. It should also be noted that the amygdala is very important to assessing the emotional experiences of memory.
Cognition is another important feature of brain function. Cognition means reception and perception of perceived stimuli and its interpretation, which includes learning, decision making, attention, and judgment. Similar to memory, cognition is mainly formed in the hippocampus, amygdala, and temporal lobe. The net effect of stress on cognition is a reduction in cognition and thus, it is said that any behavioral steps undertaken to reduce stress leads to increase in cognition. Activation of stress results in the production and release of glucocorticosteroids. Because of the lipophilic properties of glucocorticosteroids, they can diffuse through the blood-brain barrier and exert long-term effects on processing and cognition.
Memory is one of the important functional aspects of the CNS. Short term memory is dependent on the function of the frontal and parietal lobes, while long-term memory depends on the function of large areas of the brain. However, total function of memory and the conversion of short-term memory to long-term memory are dependent on the hippocampus; an area of the brain that has the highest density of glucocorticosteroid receptors and also represents the highest level of response to stress. It should also be noted that the amygdala is very important to assessing the emotional experiences of memory.
Cognition is another important feature of brain function. Cognition means reception and perception of perceived stimuli and its interpretation, which includes learning, decision making, attention, and judgment. Similar to memory, cognition is mainly formed in the hippocampus, amygdala, and temporal lobe. The net effect of stress on cognition is a reduction in cognition and thus, it is said that any behavioral steps undertaken to reduce stress leads to increase in cognition. Activation of stress results in the production and release of glucocorticosteroids. Because of the lipophilic properties of glucocorticosteroids, they can diffuse through the blood-brain barrier and exert long-term effects on processing and cognition.
stress and the immune system
Stress can affect the function of the immune system by modulating processes in the CNS and neuroendocrine system.
- Stress triggers release of corticotropin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), and cortisol. This weakens the immune response.
- Secretion of growth hormone will be halted during severe stress.
- GH is known to promote immune function such as stimulation of T and B cell proliferation.
- Severe stress can lead to malignancy by suppressing the immune system (10).
- Can decrease the activity of cytotoxic T lymphocytes and natural killer cells and lead to growth of malignant cells and tumor expansion.
- Stress has also been associated with exacerbations of autoimmune disease (11)
- They argue that immune cells become “resistant” to the effects of cortisol primarily through a reduction, or downregulation, in the number of expressed cortisol receptors (12).
- With cortisol unable to suppress inflammation, stress continues to promote proinflammatory cytokine production indefinitely (12).
stress and the cardiovascular system
Stress, whether acute or chronic, has a deleterious effect on the function of the cardiovascular system.
- Activation of the sympathetic nervous system mainly results in an increase in heart rate, strength of contraction, vasodilation in the arteries of skeletal muscles, a narrowing of the veins, contraction of the arteries in the spleen and kidneys, and decreased sodium excretion by the kidneys (13).
- Sometimes, stress activates the parasympathetic nervous system (sympathovagal interaction). Specifically, if it leads to stimulation of the limbic system, it results in a decrease, or even a total stopping of the heart-beat, decreased contractility, arrhythmia, peripheral vasodilatation, and a decline in blood pressure (14, 15).
- Stress can modulate vascular endothelial cell function and increase the risk of thrombosis and ischemia, as well as increase platelet aggregation (16).
- Psychological stress can cause alpha-adrenergic stimulation and as a result, coronary vasoconstriction is enhanced, which may increase the risk of myocardial infarction (16).
- Women begin to exhibit heart disease ten years later than men, which has been attributed to the protective effects of the estrogen hormone (16).
- The protection against cardiovascular disease in women during reproductive age is believed to be related at least in part to estradiol (E2).
- E2 mediates its cardioprotective actions by increasing angiogenesis and vasodilation and decreasing reactive oxygen species, oxidative stress, and fibrosis. Through these mechanisms, E2 limits cardiac remodeling and attenuates heart hypertrophy (24).
stress and the gastrointestinal system
The effects of stress on nutrition and the gastrointestinal (GI) system can be summarized with two aspects of GI function.
1.Stress can affect appetite
1.Stress can affect appetite
- Related to involvement of either the ventral tegmental area (VTA), or the amygdala via N-methyl-D-aspartate (NMDA) glutamate receptors (17).
- Studies have shown that stress affects the absorption process, intestinal permeability, mucus and stomach acid secretion, function of ion channels, and GI inflammation (18).
- Prevents stomach emptying and accelerates colon movement (22)
- Stress also increases the response of the GI system to inflammation and may reactivate previous inflammation and accelerate the inflammation process by secretion of mediators such as substance P (18).
- Many inflammatory diseases, such as Crohn's disease and other ulcerative-based diseases of the GI tract, are associated with stress. (19) It has been suggested that even childhood stress can lead to these diseases in adulthood (20).
- Irritable bowel syndrome, which is a disease with an inflammatory origin, is highly related to stress (21).
stress and the endocrine system
Stress can either activate, or change the activity of, many endocrine processes associated with the hypothalamus, pituitary and adrenal glands, the adrenergic system, gonads, thyroid, and the pancreas.
Article Review
The Impact of Stress on Body Functions
Psychological Stress and the Human Immune System
- Even a minimal amount of stress can activate the hypothalamic-pituitary-adrenal axis, which itself is intricately involved with the activation of several different hormone secreting systems (23).
Article Review
The Impact of Stress on Body Functions
Psychological Stress and the Human Immune System
In conclusion, stress may produce both beneficial and harmful effects. The beneficial effects are the preservation of homeostasis within the human body and the concerted efforts towards survival. However, the harmful effects of stress has received more attention because of their role in promoting illnesses. Many disorders stem from stress, especially if the stress is severe and prolonged. Thus, the medical community needs to have greater awareness and appreciation for the significant role of stress in the pathophysiology of diseases and treat them accordingly using both pharmacological and non-pharmacological interventions such as change in lifestyle, exercise, healthy diet, and stress reduction programs. The physician must also remember that response to stress will vary by individual, thus management needs to be tailored according to the person.
In conclusion, stress may produce both beneficial and harmful effects. The beneficial effects are the preservation of homeostasis within the human body and the concerted efforts towards survival. However, the harmful effects of stress has received more attention because of their role in promoting illnesses. Many disorders stem from stress, especially if the stress is severe and prolonged. Thus, the medical community needs to have greater awareness and appreciation for the significant role of stress in the pathophysiology of diseases and treat them accordingly using both pharmacological and non-pharmacological interventions such as change in lifestyle, exercise, healthy diet, and stress reduction programs. The physician must also remember that response to stress will vary by individual, thus management needs to be tailored according to the person.
TASKS |
REFLECTIVE JOURNAL Now that you have learned more about the contributions of stress in our society and how it affects us, share your reflections on this topic (including the article reviews). CASE PRESENTATION Search for a published case on the effect of Stress on Health and record a case presentation. |
References:
- Selye H. The Stress of Life. New York: McGraw-Hill; 1956.
- Dhabhar FS, McEwen BS. Acute stress enhances while chronic stress suppresses cell-mediated immunity in vivo: a potential role for leukocyte trafficking. Brain Behav Immun. 1997 Dec; 11(4):286-306.
- Llabre MM, Klein BR, Saab PG, McCalla JB, Schneiderman N. Classification of individual differences in cardiovascular responsivity: the contribution of reactor type controlling for race and gender. Int J Behav Med. 1998; 5(3):213-29.
- Dhabhar FS, McEwen BS. Acute stress enhances while chronic stress suppresses cell-mediated immunity in vivo: a potential role for leukocyte trafficking. Brain Behav Immun. 1997 Dec; 11(4):286-306.
- Henry JP, Stephens PM, Santisteban GA. A model of psychosocial hypertension showing reversibility and progression of cardiovascular complications. Circ Res. 1975 Jan; 36(1):156-64.
- Brownley KA, Hurwitz BE, Schneiderman N. Cardiovascular psychophysiology. In: Cacioppo JT, Tassinary LG, Berntson GG, editors. Handbook of Psychophysiology. 2nd ed. New York: Cambridge Univ.; 2000. pp. 224–264.
- Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004 Jul; 130(4):601-30.
- Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology: psychological influences on immune function and health. J Consult Clin Psychol. 2002 Jun; 70(3):537-47.
- Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: A review. EXCLI J. 2017;16:1057-1072. Published 2017 Jul 21. doi:10.17179/excli2017-480
- Reiche EM, Nunes SO, Morimoto HK. Stress, depression, the immune system, and cancer. Lancet Oncol. 2004 Oct; 5(10):617-25.
- Harbuz MS, Chover-Gonzalez AJ, Jessop DS. Hypothalamo-pituitary-adrenal axis and chronic immune activation. Ann N Y Acad Sci. 2003 May; 992():99-106.
- Miller GE, Cohen S, Ritchey AK. Chronic psychological stress and the regulation of pro-inflammatory cytokines: a glucocorticoid-resistance model. Health Psychol. 2002 Nov; 21(6):531-41.
- Herd JA. Cardiovascular response to stress. Physiol Rev. 1991 Jan; 71(1):305-30.
- Pagani M, Mazzuero G, Ferrari A, Liberati D, Cerutti S, Vaitl D, Tavazzi L, Malliani A. Sympathovagal interaction during mental stress. A study using spectral analysis of heart rate variability in healthy control subjects and patients with a prior myocardial infarction. Circulation. 1991 Apr; 83(4 Suppl):II43-51.
- Cohen H, Benjamin J, Geva AB, Matar MA, Kaplan Z, Kotler M. Autonomic dysregulation in panic disorder and in post-traumatic stress disorder: application of power spectrum analysis of heart rate variability at rest and in response to recollection of trauma or panic attacks. Psychiatry Res. 2000 Sep 25; 96(1):1-13.
- Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999 Apr 27; 99(16):2192-217.
- Nasihatkon ZS, Khosravi M, Bourbour Z, Sahraei H, Ranjbaran M, Hassantash SM, Sahraei M, Baghlani K. Inhibitory effect of NMDA receptors in the ventral tegmental area on hormonal and eating behavior responses to stress in rats. Behav Neurol. 2014; 2014():294149.
- Collins SM. Stress and the Gastrointestinal Tract IV. Modulation of intestinal inflammation by stress: basic mechanisms and clinical relevance. Am J Physiol Gastrointest Liver Physiol. 2001 Mar; 280(3):G315-8.
- Hommes D, van den Blink B, Plasse T, Bartelsman J, Xu C, Macpherson B, Tytgat G, Peppelenbosch M, Van Deventer S. Inhibition of stress-activated MAP kinases induces clinical improvement in moderate to severe Crohn's disease. Gastroenterology. 2002 Jan; 122(1):7-14.
- Schwartz RA, Schwartz I. Psychiatric disorders associated with Crohn's disease. Int J Psychiatry Med. 1982; 12(1):67-73.
- Gonsalkorale WM, Perrey C, Pravica V, Whorwell PJ, Hutchinson IV. Interleukin 10 genotypes in irritable bowel syndrome: evidence for an inflammatory component?. Gut. 2003 Jan; 52(1):91-3.
- Mönnikes H, Tebbe J, Hildebrandt M, Arck P, Osmanoglou E, Rose M, et al. Role of stress in functional gastrointestinal disorders. Digest Dis. 2001;19:201–211.
- Sapolsky RM. Endocrinology of the stress-response. In: Becker JB, Breedlove SM, Crews D, McCarthy MM, editors. Behavioral endocrinology. 2nd. Cambridge, MA: MIT Press; 2002. pp. 409
- Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. 2017;8(1):33. Published 2017 Oct 24. doi:10.1186/s13293-017-0152-8