MODULE 4 - Lifestyle Medicine Clinical Processes (Part 2) |
|
Objectives:
|
lifestyle medicine practice model
Healthy behavior counseling has been part of the guidelines and recommendations for chronic disease. However, it's intentional implementation in the clinical set up is yet to be developed by health care providers.
Integration of healthy behaviors in primary care has been studied in many areas of the world. The Prescription for Health awarded 27 grants to Practice-Based Research Networks (PBRN) between 2003 and 2007 to test the feasibility of implementing innovative strategies for improving the reach and practicality of behavior change counseling in primary care practice. There were 22 primary care practice-based research networks developed, tested with strategies targeted on the four health risk factors:
Integration of healthy behaviors in primary care has been studied in many areas of the world. The Prescription for Health awarded 27 grants to Practice-Based Research Networks (PBRN) between 2003 and 2007 to test the feasibility of implementing innovative strategies for improving the reach and practicality of behavior change counseling in primary care practice. There were 22 primary care practice-based research networks developed, tested with strategies targeted on the four health risk factors:
- Tobacco use
- Risky alcohol use
- Unhealthy diet
- Physical inactivity
Below are some evidence-based tools you can use as reference to integrate lifestyle medicine intervention in your clinical practice:
LEAP Booklet
Effect on Delivery of 5As
Health Teens Counseling Approach
Community Health Educator Referral
Modular Lifestyle Intervention Tool
Tips:
- Implement your customized office flow based on the services you intend to provide that effectively identify and address patient's needs
- Utilize available mobile apps and other software that can track lifestyle change progress and prompt lifestyle interventions
- Constantly review patient registries and assessment to identify patients in need of intensive lifestyle interventions
- Incorporate office tools with shared medical appointments
assess and improve quality of service
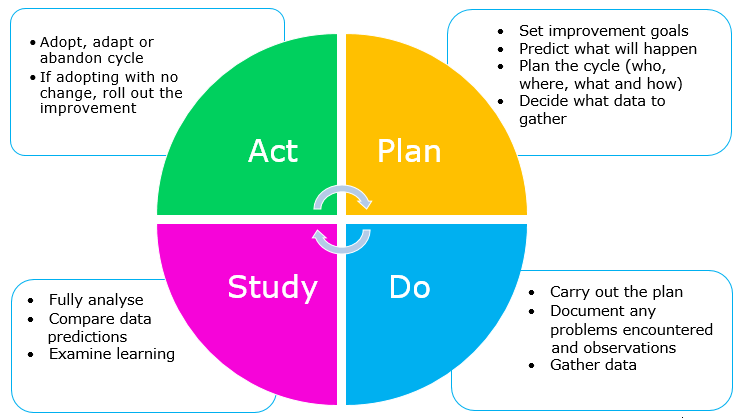
In a collaborative practice model, you have to assure that the health care team members routinely plan, conduct, and evaluate clinical processes and intervention outcome. It is a crucial process that should not be neglected in a lifestyle medicine center. Improvement methodologies are used internationally to improve intervention processes and patient outcomes. Clinical Practice Improvement (CPI) is a commonly used methodology to address identified problems in the clinical area. It involves identifying, defining and diagnosing a problem, before developing solutions and implementing interventions that may address the identified issues. Possible solutions are then tested using small-cycle testing called "Plan, Do, Study, Act" (PDSA) cycles (Nolan T 2004) with the following leading questions:
QUALITY
- What specific change are you trying to accomplish in your practice?
- How will you know that the change is an improvement?
- What adjustments to the initial change do you need to make to achieve the improvement?
QUALITY
- The capacity of the elements of that care to achieve legitimate medical and nonmedical goals.
- Tools that help us measure or quantify health care processes, outcomes, patient perceptions, and organizational structure and/or systems.
- Ongoing measurement and improvement interventions
- Flexible team - to adjust roles and procedures based on measurement results
- Team open to innovations
EXAMPLE:
What do we want to improve?
- The capture of lifestyle vital signs
- Test capture of data by medical assistant above the SOAP note in the medical record remarked with all lifestyle vital sign elements
- Provider will check for this data at the beginning of the encounter
- At least 90% of charts will contain this data (some patients may refuse or provide incomplete responses)
The theory is that having a written prompt, as well as having both the assistant and the provider check the data - will increase completeness of data. PDSA requires the following:
- Quick planning
- Small tests of change
- Iterative process over several cycles
- Planned and structured time to look at clinic processes, learn from each cycle and plan the next one
RAPID CYCLE IMPROVEMENT: PLAN
- Capture of lifestyle vital signs
RAPID CYCLE IMPROVEMENT: DO
Map the Process Flow
- Patient arrives --- checked in by front office staff (insurance/billing) --- patient is take to the exam room by assistant who will get the lifestyle vital signs along with standard vital signs --- assistant notates the data in the chart (paper or electronic) --- provider checks the chart and completes any missing information
- Do above process with every patient on one clinic day
- Collect the chart for all patients that day; enter results on a tracking log (all vitals captured for each patient)
RAPID CYCLE IMPROVEMENT: STUDY
Evaluate and determine the success rate
Evaluate and determine the success rate
- Review the number of vitals collected from total patients seen; calculate percent completeness; interview assistant and provided about the process and what went well and what needs improvement.
- If the result shows that vitals were only 70% complete, compare what occurred with patients whose vitals were complete and those whose vitals were not; you notice that the patients whose vitals were incomplete were at the end of the day when you were running late.
RAPID CYCLE IMPROVEMENT: ACT
Adopt by testing on a larger scale
Adapt based on lessons learned
Abandon by trying something different
Adopt by testing on a larger scale
Adapt based on lessons learned
Abandon by trying something different
- You decide to ask patients to answer to answer lifestyle vital signs questions on a form in process in the waiting room to give the medical assistant time to review the chart.
steps in clinic flow
- Initial comprehensive visit should include an inquiry about community services the patient is already accessing and the need of assessment for additional services.
- During the treatment and action planning, discuss with the patient needed support services
- A team member should review any lifestyle medicine treatment prescriptions and action plans and provide list of needed community resources on patient "discharge" from the visit.
- During subsequent visits, the need for assessment and community referral list provided should be updated as needed, specifically when treatment and action plans change.
Tools and information resources for your lifestyle medicine practice is as important as using your stethoscope. Without these tools, you will least likely able to implement effective lifestyle assessment and intervention. Efficient tolls are designed with the following tool characteristics:
- Easy to use
- Every visit
- Engages patient
- Useful for tracking
- Practical - useful for daily living
- Applicable across all domains of life - home, work, medical settings
- "Dashboard" - at-a-glance view of what is working well and what needs attention
- Universal - standard throughout healthcare
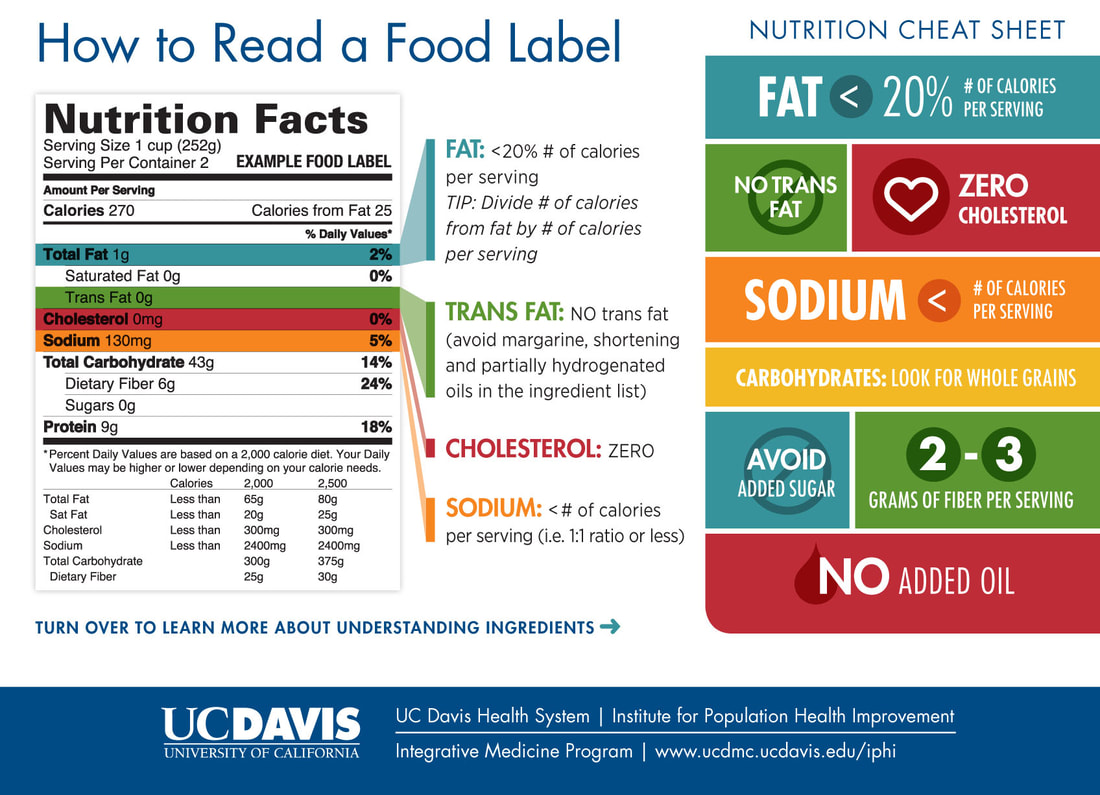
Below are resources that you can use as reference as you create your own customized forms and flier that can be given to patients as take home materials.
LIFESTYLE MEDICINE PRACTICE MODEL
SUMMARY
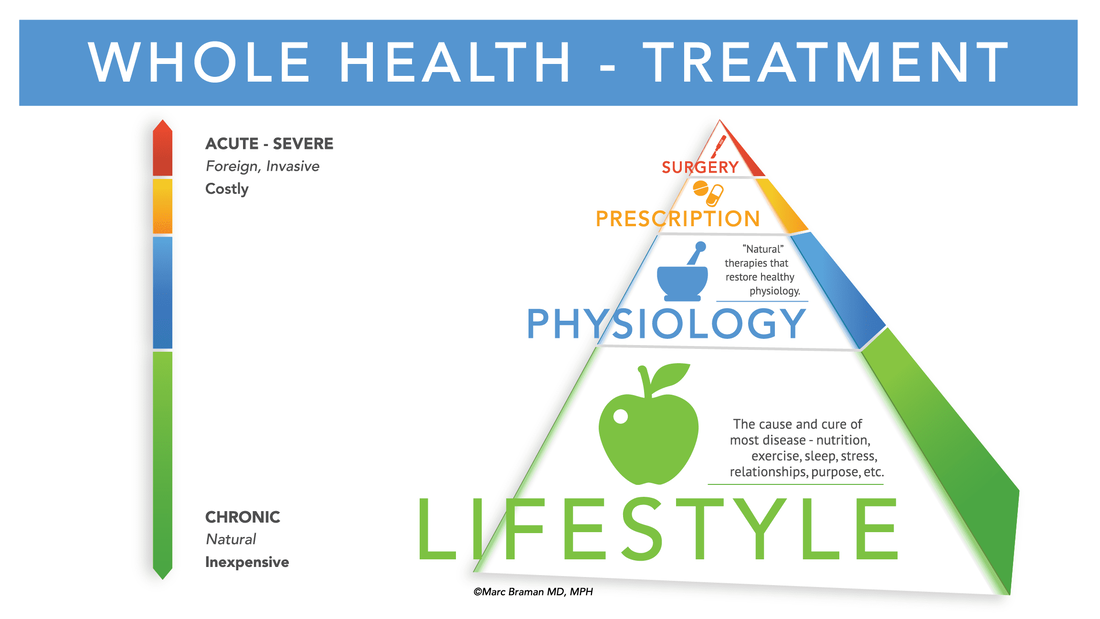
- Evaluate a patient's current health status in the context of their life journey.
- Use effective health assessment tools for a proper whole person Lifestyle Medicine diagnosis and treatment plan, not only physical conditions or "downstream" behaviors
- Utilize a consistent lifestyle "vital signs" system. Lifestyle "vital signs" are the basic metrics of lifestyle medicine and should be understood in the context of how they relate to each other.
- Recognize the role of emotional health status of patients seeking medical care. Stress and one's emotional state are often the most direct drivers of lifestyle behaviors and are often a large factor in those seeking healthcare services.
- Empower patients to actively engage in their health care. Conduct the lifestyle medicine oriented history and physical exam with the objective to support valued and empowered patient.
- Use office systems specifically to facilitate a team-based model of care. New models of care use the team approach in all medical settings, not only lifestyle medicine practices.
- Implement office systems that enhance lifestyle-based patient care. Office systems should enable the provision of effective patient-centric clinical care, such as group visits and digital technology.
- Utilize decision support technology and engagement support technology. Decision and engagement support technology and systems can facilitate desired outcome.
- Use practice guidelines well and in accordance with Lifestyle Medicine principles and evidence-base. National practice guidelines generally align with and can be adapted as needed, according to lifestyle medicine principles and its evidence-base.
- Leverage the lifestyle medicine components of practice guidelines. The trend of practice guidelines increasingly reflects lifestyle medicine foundational principles.
- Use condition-based guidelines for specific patients. Some practice guidelines are developed based on conditions and diagnoses.
- Refer to lifestyle-based guidelines when working with patients. Some practice guidelines are developed based on lifestyle modalities, including nutrition, physical activity and addressing tobacco use.
- Treat the patient, not the guidelines. Emphasize patient-focused care v.s. guidelines-focused care.
- Describe key quality promotion approaches and their origins and purposes. Quality improvement processes drive the best lifestyle medicine outcomes.
- Identify the forces affective quality and outcomes for lifestyle medicine and effectively apply/embrace them. Quality processes in a rapidly changing healthcare environment include digital technology, big date, artificial intelligence and more.
- Apply PDSA processes for quality improvement in lifestyle medicine outcomes. Using Plan-Do-Study-Act (PDSA) is one of the most common and useful quality improvement processes.
- Apply root cause analysis for quality improvement in lifestyle medicine outcomes. Using root cause analysis as a method of identifying causative factors in a process or situation e.g. Lifestyle Medicine nonadherence.
- Apply process mapping for quality improvement in lifestyle medicine outcomes. Using process mapping is a useful tool approach to understand a process and how components relate or flow.
TASK - Clinical Application |
Step 1 Using the reference provided in this module, create your own SMART goal worksheet and attach it in your lifestyle intake form. Step 2 Print the information materials provided (Dietary fiber assessment, reading food labels, etc.) and prepare them for distribution during patient's visit. Step 3 Use the forms to at least 3 of your patients (old/new) who have chronic disease and provide them the information materials as take home monitoring guide. Step 4 Ask patient's feedback on the new clinical process you have integrated in your regular clinic visit. Step 5 Compose your reflective journal on the topics covered. |