EMOTIONAL AND MENTAL HEALTH - MODULE 1 |
Lifestyle medicine health care providers should take an active role in screening, diagnosing, treating, and referring for mental health and emotional well-being. You should be able to identify components of emotional wellness self-management, facilitate lifestyle interventions to promote emotional well-being and apply positive psychology in a lifestyle medicine setting. But before discussing on self-management techniques and other key coping skills, it is necessary to take a brief review on neuropsychology.
neurophysiology
MONOAMINE NEUROTRANSMITTERS
The monoamine neurotransmitters and acetylcholine have been historically implicated in the pathophysiology and treatment of a wide variety of neuropsychiatric disorders.
Serotonin
Although only one in a million CNS neurons produces serotonin, these cells influence virtually all aspects of the CNS function. The cell bodies of these serotonergic neurons are clustered in the midline raphe nuclei of the brainstem; it also sends ascending axonal projections throughout the brain and descending projections into the medulla, cerebellum, and spinal cord. The descending serotonergic fibers that innervate the dorsal horn of the spinal cord have been implicated in the suppression of nociceptive pathways – can explain the pain-relieving effects of serotonin. The firing of the CNS serotonin neurons varies across the sleep-wake cycle, with an absence of activity during rapid eye movement (REM) sleep. Increased firing is observed during rhythmic motor behaviors and suggests that serotonin modulates some forms of motor output.
Most serotonergic innervation of the cortex and limbic system come from the dorsal and median raphe nuclei in the midbrain. The median raphe provides most of the serotonergic fibers that innervate the limbic system, whereas the dorsal raphe nucleus provides most of the serotonergic fibers that innervate the striatum and thalamus.
Clinical Correlation
The monoamine neurotransmitters and acetylcholine have been historically implicated in the pathophysiology and treatment of a wide variety of neuropsychiatric disorders.
Serotonin
Although only one in a million CNS neurons produces serotonin, these cells influence virtually all aspects of the CNS function. The cell bodies of these serotonergic neurons are clustered in the midline raphe nuclei of the brainstem; it also sends ascending axonal projections throughout the brain and descending projections into the medulla, cerebellum, and spinal cord. The descending serotonergic fibers that innervate the dorsal horn of the spinal cord have been implicated in the suppression of nociceptive pathways – can explain the pain-relieving effects of serotonin. The firing of the CNS serotonin neurons varies across the sleep-wake cycle, with an absence of activity during rapid eye movement (REM) sleep. Increased firing is observed during rhythmic motor behaviors and suggests that serotonin modulates some forms of motor output.
Most serotonergic innervation of the cortex and limbic system come from the dorsal and median raphe nuclei in the midbrain. The median raphe provides most of the serotonergic fibers that innervate the limbic system, whereas the dorsal raphe nucleus provides most of the serotonergic fibers that innervate the striatum and thalamus.
Clinical Correlation
- Current hypotheses posit serotonin excess as a cause of both positive and negative symptoms in schizophrenia.
- The biogenic amine neurotransmitter most commonly associated with depression. Depletion of serotonin may precipitate depression.
Dopamine
Dopamine neurons are more widely distributed than those of other monoamines. They reside in the midbrain substantia nigra and ventral tegmental area and in the periaqueductal gray, hypothalamus, olfactory bulb, and retina. In the periphery, dopamine is found in the kidney where it functions to produce renal vasodilation, diuresis, and natriuresis. Three dopamine systems are highly relevant to psychiatry: the nigrostriatal, mesocorticolimbic, and tuberohypophyseal system. The nigrostriatal system modulate motor control and degeneration causes Parkinson’s disease. The extrapyramidal effects of antipsychotic drugs are thought from the blockade of this system as well.
The mesocorticolimbic dopamine pathway is central in the representation of reward.
Clinical Correlation
Norepinephrine and Epinephrine
The postganglionic sympathetic neurons of the autonomic nervous system release norepinephrine, resulting in widespread peripheral effects including tachycardia and elevated blood pressure. The adrenal medulla releases epinephrine, which produces similar effects.
Norepinephrine-producing neurons are found within the brain in the pons and medulla. Projections from these regions reach the neocortex, hippocampus, thalamus, and midbrain tectum. Firing rates are responsive to stressful stimuli. Studies indicate their role in the regulation of arousal state, vigilance, and stress response.
Clinical Correlation
Acetylcholine
Two large clusters of cholinergic projection neurons are found within the brain: the basal forebrain complex and the mesopontine complex. In Alzheimer’s disease there is significant reduction in cortical cholinergic innervation. The extent of neuronal loss correlates with the degree of dementia. In contrast to central serotonergic, noradrenergic, and histaminergic neurons, cholinergic neurons may continue to fire during REM sleep and have been proposed to play a role in REM sleep induction. Peripheral acetylcholine mediates the effects of the parasympathetic system, including bradycardia and reduced blood pressure, and enhanced digestive function.
Clinical Correlation
AMINO ACID NEUROTRANSMITTERS
Glutamic Acid mediates fast excitatory neurotransmission in the brain and is the transmitter for approximately 80% of brain synapses.
Clinical Correlation
Inhibitory Amino Acids: GABA is the major inhibitory neurotransmitter in the brain, where it is broadly distributed. GABA is synthesized from glutamic acid.
Clinical Correlation
Dopamine neurons are more widely distributed than those of other monoamines. They reside in the midbrain substantia nigra and ventral tegmental area and in the periaqueductal gray, hypothalamus, olfactory bulb, and retina. In the periphery, dopamine is found in the kidney where it functions to produce renal vasodilation, diuresis, and natriuresis. Three dopamine systems are highly relevant to psychiatry: the nigrostriatal, mesocorticolimbic, and tuberohypophyseal system. The nigrostriatal system modulate motor control and degeneration causes Parkinson’s disease. The extrapyramidal effects of antipsychotic drugs are thought from the blockade of this system as well.
The mesocorticolimbic dopamine pathway is central in the representation of reward.
Clinical Correlation
- Drugs of abuse activate the mesocorticolimbic pathway, and plastic changes in this pathway are thought to underlie drug addiction.
- Schizophrenia is hypothesized to result from too much dopaminergic activity.
- Dopamine may be reduced in depression and increased in mania.
Norepinephrine and Epinephrine
The postganglionic sympathetic neurons of the autonomic nervous system release norepinephrine, resulting in widespread peripheral effects including tachycardia and elevated blood pressure. The adrenal medulla releases epinephrine, which produces similar effects.
Norepinephrine-producing neurons are found within the brain in the pons and medulla. Projections from these regions reach the neocortex, hippocampus, thalamus, and midbrain tectum. Firing rates are responsive to stressful stimuli. Studies indicate their role in the regulation of arousal state, vigilance, and stress response.
Clinical Correlation
- Selective neuronal degeneration within the norepinephrine reward neuronal system could account for anhedonia.
- Depression: downregulation or decreased sensitivity of β-adrenergic receptors
- Chronic symptoms experienced by patients with anxiety disorder, such as panic attacks, insomnia, startle, and autonomic hyperarousal, are characteristic of increased noradrenergic function.
Acetylcholine
Two large clusters of cholinergic projection neurons are found within the brain: the basal forebrain complex and the mesopontine complex. In Alzheimer’s disease there is significant reduction in cortical cholinergic innervation. The extent of neuronal loss correlates with the degree of dementia. In contrast to central serotonergic, noradrenergic, and histaminergic neurons, cholinergic neurons may continue to fire during REM sleep and have been proposed to play a role in REM sleep induction. Peripheral acetylcholine mediates the effects of the parasympathetic system, including bradycardia and reduced blood pressure, and enhanced digestive function.
Clinical Correlation
- Increased Ach can produce lethargy, anergia, and psychomotor retardation in healthy subjects, can exacerbate symptoms in depression, and can reduce symptoms in mania.
AMINO ACID NEUROTRANSMITTERS
Glutamic Acid mediates fast excitatory neurotransmission in the brain and is the transmitter for approximately 80% of brain synapses.
Clinical Correlation
- Glutamate bind to sites associated with the N-methyl-D-aspartate (NMDA) receptor, and excessive glutamatergic stimulation can cause neurotoxic effects.
- A high concentration of NMDA receptors exists in the hippocampus. Glutamate, thus, may work in conjunction with hypercortisolemia to mediate the deleterious neurocognitive effects of severe recurrent depression.
Inhibitory Amino Acids: GABA is the major inhibitory neurotransmitter in the brain, where it is broadly distributed. GABA is synthesized from glutamic acid.
Clinical Correlation
- Schizophrenia: loss of GABAergic neurons in the hippocampus; loss of inhibitory GABAergic neurons could lead to the hyperactivity of dopaminergic neurons.
- Reduced levels of GABA in depression.
- Chronic stress can reduce and eventually deplete GABA levels.
- Some patients with anxiety disorders may have abnormal functioning of their GABAA receptors.
psychoneuroendocrinology
Psychoneuroendocrinology encompasses the structural and functional relationships between hormonal systems and the CNS and behaviors.
HPA Axis
Hormone secretion is stimulated by the action of a neuronal secretory product of the hypothalamus (eg. coricotropin-releasing hormone which stimulates adrenocorticotropic hormone). Chemical signals cause the release of these neurohormones from the hypothalamus to the portal hypophyseal bloodstream and is transported to the pituitary to regulate the release of target hormones. Pituitary hormones in turn act directly on target cells (e.g., ACTH on the adrenal gland) or stimulate the release of other hormones from peripheral endocrine organs. In addition, these hormones have feedback actions to regulate secretion and exert neuromodulatory effects in the CNS.
Since the earliest conceptions of the stress response, by Hans Selye and others, investigation of hypothalamic-pituitary-adrenal (HPA) function has occupied a central position in psychoendocrine research. CRH, ACTH, and cortisol levels all rise in response to a variety of physical and psychic stresses and serve as prime factors in maintaining homeostasis and developing adaptive responses to novel or challenging stimuli. The hormonal response depends both on the characteristics of the stressor itself and on how the individual assesses and is able to cope with it. Aside from generalized effects on arousal, distinct effects on sensory processing, stimulus habituation and sensitization, pain, sleep, and memory storage and retrieval have been documented.
Pathological alterations in HPA function have been associated primarily with mood disorders, posttraumatic stress disorder (PTSD), and dementia of the Alzheimer’s type. Disturbances of mood are found in more than 50% of patients with Cushing’s syndrome (characterized by elevated cortisol concentrations), with suicidal thought or psychosis apparent in more than 10% of patients studied. Cognitive impairments similar to those seen in major depressive disorder (principally in visual memory and higher cortical functions) are common and related to the severity of the hypercortisolemia and possible reduction in hippocampal size. In general, reduced cortisol levels normalize mood and mental status. Conversely, in Addison’s disease (characterized by adrenal insufficiency), apathy, social withdrawal, impaired sleep, and decreased concentration frequently accompany prominent fatigue. Replacement of glucocorticoid resolves behavioral symptomatology. Alterations in HPA function associated with depression include elevated cortisol concentrations, failure to suppress cortisol in response to dexamethasone, increased adrenal size and sensitivity to ACTH, a blunted ACTH response to CRH, and, possibly, elevated CRH concentrations in the brain.
Hypothalamic-Pituitary-Gonadal Axis
The gonadal hormones (progesterone, androstenedione, testosterone, estradiol, and others) are steroids that are secreted principally by the ovary and testes, but significant amounts of androgens arise from the adrenal cortex as well. The prostate gland and adipose tissue, also involved in the synthesis and storage of dihydrotestosterone, contribute to individual variance in sexual function and behavior.
Gonadal hormones appear to direct the organization of CNS structures and functions, such as the size of the hypothalamic nuclei and corpus callosum. Women with congenital adrenal hyperplasia, which leads to high exposure to adrenal androgens in early life, have been found to be more aggressive and assertive and less interested in traditional female roles than control female subjects.
Testosterone
Testosterone is the primary androgenic steroid. It is associated with increased violence and aggression in animals and in correlation studies in humans. In hypogonadal men, testosterone improves mood and decreases irritability. A prospective, placebo-controlled study of anabolic-androgenic steroid administration in normal subjects reported positive mood symptoms, including euphoria, increased energy, and sexual arousal, in addition to increases in the negative mood symptoms of irritability, mood swings, violent feelings, anger, and hostility.
Dehydroepiandosterone
DHEA and DEAH sulfate (DHEA-S) are adrenal androgens secreted in response to ACTH and represent the most abundant circulating steroids. DHEA is also a neurosteroid that is synthesized in situ in the brain. DHEA has many physiological effects, including reduction in neuronal damage from glucocorticoid excess and oxidative stress. Behavioral interest has centered on its possible involvement in memory, mood, and a number of psychiatric disorders. Adrenarche is the prepubertal onset of adrenal production of DHEA-S and may play a role in human maturation through increasing the activity of the amygdala and hippocampus and promoting synaptogenesis in the cerebral cortex. Several trials of DHEA administration point to an improvement in well-being, mood, energy, libido, and functional status in depressed individuals.
Animal studies suggest that DHEA may be involved in eating behavior, aggressiveness, and anxiety as well, with its effects resulting from its transformation into estrogen, testosterone, or androsterone, from its anti-glucocorticoid activity or from direct effects on GABAA, N-methyl-D-aspartate (NMDA), and σ receptors. Because of the putative anti-glucocorticoid effects, the ratio of cortisol to DHEA levels may be particularly important in understanding adaptive responses to stress. Both cortisol and DHEA appear to be involved in fear conditioning, with the cortisol/DHEA ratio hypothesized to be an index of the degree to which an individual is buffered against the negative effects of stress. Fear-potentiated startle is larger in individuals with high as compared to low cortisol/DHEA-S ratios and is positively associated with cortisol and negatively with DHEA-S.
Estrogen and Progesterone
Estrogens can influence neural activity in the hypothalamus and limbic system directly through modulation of neuronal excitability, and they have complex multiphasic effects on nigrostriatal dopamine receptor sensitivity. Several studies have suggested that gonadal steroids modulate spatial cognition and verbal memory and are involved in impeding age-related neuronal degeneration. Increasing evidence also suggests that estrogen administration decreases the risk and severity of dementia of the Alzheimer’s type in postmenopausal women. Estrogen has mood-enhancing properties and can also increase sensitivity to serotonin, possibly by inhibiting monoamine oxidase.
The association of these hormones with serotonin is hypothetically relevant to mood change in premenstrual and postpartum mood disturbances.
Most psychological symptoms associated with menopause are actually reported during perimenopause rather than after complete cessation of menses. Although studies suggest no increased incidence of major depressive disorder, reported symptoms include worry, fatigue, crying spells, mood swings, diminished ability to cope, and diminished libido. Hormone replacement therapy (HRT) is effective in preventive osteoporosis and reinstating energy, a sense of well-being, and libido; however, its use is extremely controversial. Studies have shown that combined estrogen-progesting drugs (e.g. Premarin) cause small increases in breast cancer, heart attack, stroke, and blood clots among menopausal women. Studies of the effects of estrogen alone in women who have had hysterectomies (because estrogen alone increases the risk for uterine cancer) are ongoing.
Hypothalamic-Pituitary-Thyroid Axis
Thyroid hormones are involved in the regulation of nearly every organ system, particularly those integral to the metabolism of food and regulation of temperature, and are responsible for optimal development and function of all body tissues. In addition to its prime endocrine function, TRH has direct effects on neuronal excitability, behavior, and neurotransmitter regulation.
Thyroid disorders can induce virtually any psychiatric symptom or syndrome, although no consistent associations of specific syndromes and thyroid conditions are found. Hyperthyroidism is commonly associated with fatigue, irritability, insomnia, anxiety, restlessness, weight loss, and emotional lability; marked impairment in concentration and memory may also be evident. Such states can progress into delirium or mania or they can be episodic. On occasion, a true psychosis develops, with paranoia as a particularly common presenting feature. In general, behavioral abnormalities resolve with normalization of thyroid function and respond symptomatically to traditional psychopharmacological regimens.
HPA Axis
Hormone secretion is stimulated by the action of a neuronal secretory product of the hypothalamus (eg. coricotropin-releasing hormone which stimulates adrenocorticotropic hormone). Chemical signals cause the release of these neurohormones from the hypothalamus to the portal hypophyseal bloodstream and is transported to the pituitary to regulate the release of target hormones. Pituitary hormones in turn act directly on target cells (e.g., ACTH on the adrenal gland) or stimulate the release of other hormones from peripheral endocrine organs. In addition, these hormones have feedback actions to regulate secretion and exert neuromodulatory effects in the CNS.
Since the earliest conceptions of the stress response, by Hans Selye and others, investigation of hypothalamic-pituitary-adrenal (HPA) function has occupied a central position in psychoendocrine research. CRH, ACTH, and cortisol levels all rise in response to a variety of physical and psychic stresses and serve as prime factors in maintaining homeostasis and developing adaptive responses to novel or challenging stimuli. The hormonal response depends both on the characteristics of the stressor itself and on how the individual assesses and is able to cope with it. Aside from generalized effects on arousal, distinct effects on sensory processing, stimulus habituation and sensitization, pain, sleep, and memory storage and retrieval have been documented.
Pathological alterations in HPA function have been associated primarily with mood disorders, posttraumatic stress disorder (PTSD), and dementia of the Alzheimer’s type. Disturbances of mood are found in more than 50% of patients with Cushing’s syndrome (characterized by elevated cortisol concentrations), with suicidal thought or psychosis apparent in more than 10% of patients studied. Cognitive impairments similar to those seen in major depressive disorder (principally in visual memory and higher cortical functions) are common and related to the severity of the hypercortisolemia and possible reduction in hippocampal size. In general, reduced cortisol levels normalize mood and mental status. Conversely, in Addison’s disease (characterized by adrenal insufficiency), apathy, social withdrawal, impaired sleep, and decreased concentration frequently accompany prominent fatigue. Replacement of glucocorticoid resolves behavioral symptomatology. Alterations in HPA function associated with depression include elevated cortisol concentrations, failure to suppress cortisol in response to dexamethasone, increased adrenal size and sensitivity to ACTH, a blunted ACTH response to CRH, and, possibly, elevated CRH concentrations in the brain.
Hypothalamic-Pituitary-Gonadal Axis
The gonadal hormones (progesterone, androstenedione, testosterone, estradiol, and others) are steroids that are secreted principally by the ovary and testes, but significant amounts of androgens arise from the adrenal cortex as well. The prostate gland and adipose tissue, also involved in the synthesis and storage of dihydrotestosterone, contribute to individual variance in sexual function and behavior.
Gonadal hormones appear to direct the organization of CNS structures and functions, such as the size of the hypothalamic nuclei and corpus callosum. Women with congenital adrenal hyperplasia, which leads to high exposure to adrenal androgens in early life, have been found to be more aggressive and assertive and less interested in traditional female roles than control female subjects.
Testosterone
Testosterone is the primary androgenic steroid. It is associated with increased violence and aggression in animals and in correlation studies in humans. In hypogonadal men, testosterone improves mood and decreases irritability. A prospective, placebo-controlled study of anabolic-androgenic steroid administration in normal subjects reported positive mood symptoms, including euphoria, increased energy, and sexual arousal, in addition to increases in the negative mood symptoms of irritability, mood swings, violent feelings, anger, and hostility.
Dehydroepiandosterone
DHEA and DEAH sulfate (DHEA-S) are adrenal androgens secreted in response to ACTH and represent the most abundant circulating steroids. DHEA is also a neurosteroid that is synthesized in situ in the brain. DHEA has many physiological effects, including reduction in neuronal damage from glucocorticoid excess and oxidative stress. Behavioral interest has centered on its possible involvement in memory, mood, and a number of psychiatric disorders. Adrenarche is the prepubertal onset of adrenal production of DHEA-S and may play a role in human maturation through increasing the activity of the amygdala and hippocampus and promoting synaptogenesis in the cerebral cortex. Several trials of DHEA administration point to an improvement in well-being, mood, energy, libido, and functional status in depressed individuals.
Animal studies suggest that DHEA may be involved in eating behavior, aggressiveness, and anxiety as well, with its effects resulting from its transformation into estrogen, testosterone, or androsterone, from its anti-glucocorticoid activity or from direct effects on GABAA, N-methyl-D-aspartate (NMDA), and σ receptors. Because of the putative anti-glucocorticoid effects, the ratio of cortisol to DHEA levels may be particularly important in understanding adaptive responses to stress. Both cortisol and DHEA appear to be involved in fear conditioning, with the cortisol/DHEA ratio hypothesized to be an index of the degree to which an individual is buffered against the negative effects of stress. Fear-potentiated startle is larger in individuals with high as compared to low cortisol/DHEA-S ratios and is positively associated with cortisol and negatively with DHEA-S.
Estrogen and Progesterone
Estrogens can influence neural activity in the hypothalamus and limbic system directly through modulation of neuronal excitability, and they have complex multiphasic effects on nigrostriatal dopamine receptor sensitivity. Several studies have suggested that gonadal steroids modulate spatial cognition and verbal memory and are involved in impeding age-related neuronal degeneration. Increasing evidence also suggests that estrogen administration decreases the risk and severity of dementia of the Alzheimer’s type in postmenopausal women. Estrogen has mood-enhancing properties and can also increase sensitivity to serotonin, possibly by inhibiting monoamine oxidase.
The association of these hormones with serotonin is hypothetically relevant to mood change in premenstrual and postpartum mood disturbances.
Most psychological symptoms associated with menopause are actually reported during perimenopause rather than after complete cessation of menses. Although studies suggest no increased incidence of major depressive disorder, reported symptoms include worry, fatigue, crying spells, mood swings, diminished ability to cope, and diminished libido. Hormone replacement therapy (HRT) is effective in preventive osteoporosis and reinstating energy, a sense of well-being, and libido; however, its use is extremely controversial. Studies have shown that combined estrogen-progesting drugs (e.g. Premarin) cause small increases in breast cancer, heart attack, stroke, and blood clots among menopausal women. Studies of the effects of estrogen alone in women who have had hysterectomies (because estrogen alone increases the risk for uterine cancer) are ongoing.
Hypothalamic-Pituitary-Thyroid Axis
Thyroid hormones are involved in the regulation of nearly every organ system, particularly those integral to the metabolism of food and regulation of temperature, and are responsible for optimal development and function of all body tissues. In addition to its prime endocrine function, TRH has direct effects on neuronal excitability, behavior, and neurotransmitter regulation.
Thyroid disorders can induce virtually any psychiatric symptom or syndrome, although no consistent associations of specific syndromes and thyroid conditions are found. Hyperthyroidism is commonly associated with fatigue, irritability, insomnia, anxiety, restlessness, weight loss, and emotional lability; marked impairment in concentration and memory may also be evident. Such states can progress into delirium or mania or they can be episodic. On occasion, a true psychosis develops, with paranoia as a particularly common presenting feature. In general, behavioral abnormalities resolve with normalization of thyroid function and respond symptomatically to traditional psychopharmacological regimens.
The psychiatric symptoms of chronic hypothyroidism are generally well recognized. Classically, fatigue, decreased libido, memory impairment, and irritability are noted, but a true secondary psychotic disorder or dementia-like state can also develop. Suicidal ideation is common, and the lethality of actual attempts is profound.
Growth Hormone
Growth hormone deficiencies interfere with growth and delay the onset of puberty. Low GH levels can result from a stressful experience. Administration of GH to individuals with GH deficiency benefits cognitive function in addition to its more obvious somatic effects, but evidence indicates poor psychosocial adaptation in adulthood for children who were treated for GH deficiency. A significant percentage of patients with major depressive disorder and dysthymic disorder may have a GH deficiency. Administration of GH to elderly men increases lean body mass and improves vigor. GH is released in pulses throughout the day, but the pulses are closer together during the first hours of sleep than at other times.
Growth Hormone
Growth hormone deficiencies interfere with growth and delay the onset of puberty. Low GH levels can result from a stressful experience. Administration of GH to individuals with GH deficiency benefits cognitive function in addition to its more obvious somatic effects, but evidence indicates poor psychosocial adaptation in adulthood for children who were treated for GH deficiency. A significant percentage of patients with major depressive disorder and dysthymic disorder may have a GH deficiency. Administration of GH to elderly men increases lean body mass and improves vigor. GH is released in pulses throughout the day, but the pulses are closer together during the first hours of sleep than at other times.
Prolactin
Since its identification in 1970, the anterior pituitary hormone prolactin has been examined as a potential index of dopamine activity and as a correlate of stress responsivity. The secretion of prolactin is under direct inhibitory regulation by dopamine neurons located in the hypothalamus.
Prolactin is primarily involved in reproductive functions. It participates in gonadal development during maturation and is stimulated by suckling for breast-feeding. Hyperprolactinemia is associated with low testosterone in men and reduced libido in men and women. In rodents, prolactin level is increased along with corticosterone in response to such stressful stimuli as immobilization, hypoglycemia, surgery, and cold exposure.
Patients with hyperprolactinemia often complain of depression, decreased libido, stress intolerance, anxiety, and increased irritability. These behavioral symptoms usually resolve in parallel with decrements in serum prolactin when surgical or pharmacological treatments are used.
Since its identification in 1970, the anterior pituitary hormone prolactin has been examined as a potential index of dopamine activity and as a correlate of stress responsivity. The secretion of prolactin is under direct inhibitory regulation by dopamine neurons located in the hypothalamus.
Prolactin is primarily involved in reproductive functions. It participates in gonadal development during maturation and is stimulated by suckling for breast-feeding. Hyperprolactinemia is associated with low testosterone in men and reduced libido in men and women. In rodents, prolactin level is increased along with corticosterone in response to such stressful stimuli as immobilization, hypoglycemia, surgery, and cold exposure.
Patients with hyperprolactinemia often complain of depression, decreased libido, stress intolerance, anxiety, and increased irritability. These behavioral symptoms usually resolve in parallel with decrements in serum prolactin when surgical or pharmacological treatments are used.
Melatonin
Melatonin, a pineal hormone, is derived from the serotonin molecule and it controls photoperiodically mediated endocrine events (particularly those of the hypothalamic-pituitary-gonadal axis). It also modulates immune function, mood, and reproductive performance and is a potent antioxidant and free-radical scavenger. Melatonin has a depressive effect on CNS excitability, is an analgesic, and has seizure-inhibiting effects in animal studies. Melatonin can be a useful therapeutic agent in the treatment of circadian phase disorders such as jet lag. Intake of melatonin increases the speed of falling asleep, as well as its duration and quality.
Insulin
Increasing evidence indicates that insulin may be integrally involved in learning and memory. Insulin receptors occur in high density in the hippocampus and are thought to help neurons metabolize glucose. Patients with Alzheimer’s disease have lower insulin concentrations in the cerebrospinal fluid (CSF) than controls, and both insulin and glucose dramatically improve verbal memory. Depression is frequent in patients with diabetes, as are indexes of impaired hormonal response to stress. It is not known if these findings represent direct effects of the disease or are secondary, nonspecific effects.
Melatonin, a pineal hormone, is derived from the serotonin molecule and it controls photoperiodically mediated endocrine events (particularly those of the hypothalamic-pituitary-gonadal axis). It also modulates immune function, mood, and reproductive performance and is a potent antioxidant and free-radical scavenger. Melatonin has a depressive effect on CNS excitability, is an analgesic, and has seizure-inhibiting effects in animal studies. Melatonin can be a useful therapeutic agent in the treatment of circadian phase disorders such as jet lag. Intake of melatonin increases the speed of falling asleep, as well as its duration and quality.
Insulin
Increasing evidence indicates that insulin may be integrally involved in learning and memory. Insulin receptors occur in high density in the hippocampus and are thought to help neurons metabolize glucose. Patients with Alzheimer’s disease have lower insulin concentrations in the cerebrospinal fluid (CSF) than controls, and both insulin and glucose dramatically improve verbal memory. Depression is frequent in patients with diabetes, as are indexes of impaired hormonal response to stress. It is not known if these findings represent direct effects of the disease or are secondary, nonspecific effects.
immune system and central nervous sytem interactions
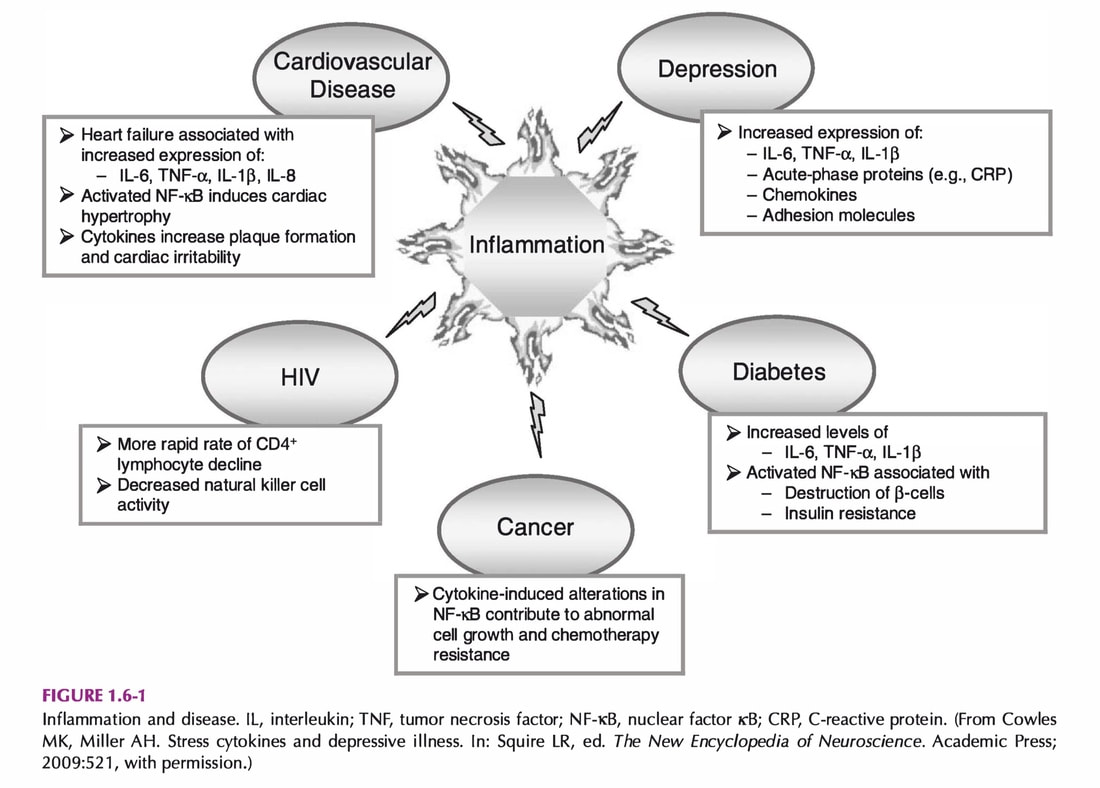
Alterations in CNS function brought about by a variety of stressors have been shown to influence the immune system. Of considerable interest is accumulating data that cytokines, which derive from immune cells and microglia, have profound effects on the CNS. The relative role of cytokines and their signaling pathways in the various psychiatric diseases is an area of active investigation, as is the role of infectious and autoimmune diseases in the pathophysiology of psychiatric disorders.
Behavioral Conditioning
The fact that learning processes are capable of influencing immunological function is an example of interactions between the immune system and the nervous system. Several classical conditioning paradigms have been associated with suppression or enhancement of the immune response in various experimental designs. The conditioning of immunological reactivity provides further evidence that the CNS can have significant immunomodulatory effects.
Stress and the Immune Response. Stress has been historically associated with suppression of immune function, but recent data indicate that stress may also activate certain aspects of the immune system, particularly the innate immune response.
Stress and Illness
The effects of stress appears to vary depending on whether it is acute or chronic, its type and severity, the timing of the stressor, and the type of tumor or infectious agent investigated. For example. Mice subjected to electric grid shock 1-3 days before the infection of Maloney murine sarcoma virus-induced tumor cells exhibited decreased tumor size and incidence. In contrast, mice exposed to grid shock 2 days after tumor cell injection exhibited an increase in tumor size and number.
The fact that learning processes are capable of influencing immunological function is an example of interactions between the immune system and the nervous system. Several classical conditioning paradigms have been associated with suppression or enhancement of the immune response in various experimental designs. The conditioning of immunological reactivity provides further evidence that the CNS can have significant immunomodulatory effects.
Stress and the Immune Response. Stress has been historically associated with suppression of immune function, but recent data indicate that stress may also activate certain aspects of the immune system, particularly the innate immune response.
Stress and Illness
The effects of stress appears to vary depending on whether it is acute or chronic, its type and severity, the timing of the stressor, and the type of tumor or infectious agent investigated. For example. Mice subjected to electric grid shock 1-3 days before the infection of Maloney murine sarcoma virus-induced tumor cells exhibited decreased tumor size and incidence. In contrast, mice exposed to grid shock 2 days after tumor cell injection exhibited an increase in tumor size and number.
|
Studies have shown an association between chronic stress and increased susceptibility to the common cold, reduced antibody responses to vaccination, and delayed wound healing. In addition, stress, as well as depression, through their effects on inflammation have been linked to increased morbidity and mortality in infectious diseases, such as HIV infection, autoimmune disorders, neoplastic diseases, as well as diabetes and cardiovascular disorders, which are increasingly being recognized as diseases in which the immune system, inflammation in particular, plays a pivotal role .
|
Effects of Chronic Stress
When challenged with a medical illness or chronic psychological stressor, complex interactions between the immune and nervous systems promote a constellation of immune-induced behavioral changes, alternatively referred to as “sickness syndrome” or “sickness behavior”. These behavioral changes include dysphoria, anhedonia, fatigue, social withdrawal, hyperalgesia, anorexia, altered sleep-wake patterns, and cognitive dysfunction. Although seen in response to an infection, the full syndrome can be reproduced in humans and laboratory animals by administration of innate immune cytokines. Blocking cytokine activity diminishes or prevents the development of sickness behavior in laboratory animals, even when such behavior develops as a result of psychological stress.
Immune-CNS Interactions
More recently, it has become evident that stress also activates inflammatory pathways, even while suppressing measures of acquired immunity. Studies now also indicate that, in addition to immunosuppression, major depression is also frequently associated with inflammatory activation.
When challenged with a medical illness or chronic psychological stressor, complex interactions between the immune and nervous systems promote a constellation of immune-induced behavioral changes, alternatively referred to as “sickness syndrome” or “sickness behavior”. These behavioral changes include dysphoria, anhedonia, fatigue, social withdrawal, hyperalgesia, anorexia, altered sleep-wake patterns, and cognitive dysfunction. Although seen in response to an infection, the full syndrome can be reproduced in humans and laboratory animals by administration of innate immune cytokines. Blocking cytokine activity diminishes or prevents the development of sickness behavior in laboratory animals, even when such behavior develops as a result of psychological stress.
Immune-CNS Interactions
More recently, it has become evident that stress also activates inflammatory pathways, even while suppressing measures of acquired immunity. Studies now also indicate that, in addition to immunosuppression, major depression is also frequently associated with inflammatory activation.
Several studies have observed that bipolar patients, especially when manic, demonstrate increased plasma concentrations of inflammatory cytokines. Of interest, the available literature seems to suggest that patients in the manic phase of the disorder may be more likely than depressed patients to demonstrate increased inflammatory markers.
Behavioral Interventions and Immunity
It has been known for years that psychosocial factors can mitigate or worsen the effects of stress, not only on immune functioning but also on the long-term outcomes of medical conditions in which the immune system is known to play a role. Therefore, behavioral interventions aimed at maximizing protective psychosocial factors might be predicted to have a beneficial effect, not only in terms of mitigating the effect of stress on immune functioning but perhaps also on diminishing emotional disturbances that arise in the context of immune system dysregulation.
Behavioral Interventions and Immunity
It has been known for years that psychosocial factors can mitigate or worsen the effects of stress, not only on immune functioning but also on the long-term outcomes of medical conditions in which the immune system is known to play a role. Therefore, behavioral interventions aimed at maximizing protective psychosocial factors might be predicted to have a beneficial effect, not only in terms of mitigating the effect of stress on immune functioning but perhaps also on diminishing emotional disturbances that arise in the context of immune system dysregulation.
Two factors that have been repeatedly identified as protective against stress-induced immune alterations are: social support and the ability to see stressors as being to some degree under the individual’s control. In this regard, a recent study that conducted a genome-wide scan to assess gene expression activity in socially isolated versus non-isolated individuals found that social isolation was associated with increased activation of a number of proinflammatory, cytokine-related pathways and reduced activity in anti-inflammatory cytokine pathways, as well as in the glucocorticoid receptor, which plays an important role in neuroendocrine control of inflammatory processes.
Of interest, the two types of psychotherapy most often examined in illnesses associated with immune dysregulation are:
Of interest, the two types of psychotherapy most often examined in illnesses associated with immune dysregulation are:
- group therapy, which provides social support, and
- cognitive behavioral therapy, which provides cognitive reframing techniques aimed at enhancing one’s sense of agency (and hence control).
VIDEO REVIEW
|
Acute Effect of Stress
|
Chronic Effect of Stress
|
Reference:
Sadock, Benjamin James, Sadock, Virginia Alcott, Ruiz, Pedro. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. 11th ed. Philadelphia, USA: Wolters Kluwer, 2015.
Sadock, Benjamin James, Sadock, Virginia Alcott, Ruiz, Pedro. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. 11th ed. Philadelphia, USA: Wolters Kluwer, 2015.
TASKS |
REFLECTIVE JOURNAL
|
Deadline for completion: September 11, 2022
VIRTUAL DISCUSSION