MODULE 2 - Key Clinical Processes in Lifestyle Medicine |
|
Objectives:
|
LM IN CLINICAL PRACTICE GUIDELINES
Over the past few decades, many scientific studies have reinforced the role of lifestyle in health and disease. Lifestyle medicine has scientifically proven research as its foundation, and a range of important worldwide studies have provided insights into the nature of disease, risk factors and the ways in which lifestyle can be modified for positive health outcomes. It has been an exciting time in health research, as discoveries have been made that can dramatically influence the course of disease, with restoration of optimal health as its goal.
Lifestyle therapy is always included in the prevention and management of chronic diseases such as atherosclerotic cardiovascular disease, hypertension, diabetes type 2, dyslipidemia, obesity and cancer. Recent data however, is showing reversal of disease and influencing even the genetic expression and overall clinical outcome of patients.
Hypertension Treatment Guideline
Prediabetes, Diabetes, Hyperlipidemia Treatment Guideline
Guideline for primary Prevention of Cardiovascular Disease
While each of the studies above, and many more, have demonstrated the role of lifestyle choices in the development or prevention of chronic diseases, other medical practitioners explored the effect of these same general principles to repair and reverse the health damage lifestyle choices may have caused to their patient's lives. It is also worth mentioning that although guidelines are showing the need for immediate implementation of lifestyle modification for patients with chronic diseases, it is least likely emphasized and intentionally prescribed in the usual clinical practice.
Diabetes Type 2 Treatment
Coronary Heart Disease Reversal
Lifestyle Modification for Obesity
Lifestyle Modification for Hypertension
lifestyle focused history & physical assessment
We have presented significant knowledge about the benefits of lifestyle medicine for prevention, management and reversal of chronic disease, but providers lack the tools necessary to convey this information to patients in an effective and efficient manner. Present barriers may include time constraints as well as lack of training and confidence in counseling patient. Further, many primary care providers have not built the interdisciplinary team and community network necessary to assist their patients or may lack the support of their health system to begin to build this structure.
This module will review provider tools for implementing Lifestyle Medicine in clinical practice. Specifically, we will review the approach to the patient, materials for teaching simple concepts in the office, learning at home activities to engage patients between visits, and clinical pearls. This will be a helpful tool for both trainees or established providers who are early in their Lifestyle Medicine career. We will address several physician competencies for prescribing Lifestyle Medicine:
- collaborate with patients to develop achievable, specific action plans
- help patients manage and sustain healthy lifestyle practices, and
- develop and apply office systems and practices to support lifestyle medical care. Equipping providers with practice tools to promote lifestyle change will improve satisfaction for patients and providers alike and is an important step toward advancing the field of a Lifestyle Medicine.
Routine check of history, physical, laboratory assessment should be routinely checked at every visit. Screening and diagnostic tests to evaluate lifestyle related risks factors and outcomes. Perform a lifestyle-related health status assessment including lifestyle "vital signs" such as:
- Nutrition
- Physical activity
- Stress
- Sleep
- Emotional well-being
- Tobacco use and Alcohol consumption
- Pain
- Environmental & occupational factors
PHYSICAL ACTIVITY ASSESSMENT
About 15-30% of typical total daily energy expenditure comes from physical activity, 10% from the thermic effect of food and about 60-75% comes from resting energy expenditure. We routinely use the global questionnaires that has good validity in classifying inactive, insufficiently active or sufficiently active individuals (Grant et al. 2014). Many patients will never know how to quantify their level of physical activity if not done intentionally during clinic visit.
About 15-30% of typical total daily energy expenditure comes from physical activity, 10% from the thermic effect of food and about 60-75% comes from resting energy expenditure. We routinely use the global questionnaires that has good validity in classifying inactive, insufficiently active or sufficiently active individuals (Grant et al. 2014). Many patients will never know how to quantify their level of physical activity if not done intentionally during clinic visit.
- How many days a week do you engage in moderate to strenuous exercise?
- On average, how many minutes per day do you exercise?
NUTRITION ASSESSMENT
The basic 24 hour food recall is the most efficient way to assess an individual's nutrition preference. Another option is to ask for a 3-day dietary log whenever applicable.
The 2015 Philippine Dietary Reference Intakes (PDRI) adopts the multi-level approach for setting nutrient reference values to meet the needs of various stakeholders for appropriate nutrient reference values. PDRI is the collective term that comprise reference value for energy and nutrient intakes used for planning and assessing diets of healthy groups and individuals. (FNRI-DOST)
- Estimated Average Requirement (EAR): daily nutrient intake level that meets the median or average requirement of healthy individuals in particular life stage and sex group, corrected for incomplete utilization or dietary nutrient bioavailability.
- Recommended Energy/Nutrient Intake (REI/RNI): level of intake of energy or nutrient which is considered adequate for the maintenance of health and well-being of healthy persons in the population.
- Adequate Intake (AI): daily nutrient intake level that is based on observed or experimentally-determined approximation of the average nutrient intake by a group of apparently healthy people that are assumed to sustain a defined nutrient state.
- Tolerable Upper Intake Level or Upper Limit (UL): highest average daily nutrient intake level likely to pose no adverse health effects to almost all individuals in the general population.
Philippine Dietary Reference Intakes 2018
CDC Guide and Strategies
USDA Dietary Guideline Advisory Committee 2015
CDC Guide and Strategies
USDA Dietary Guideline Advisory Committee 2015
According to the USDA Report Americans found to have:
- Shortfall in the following nutrients: Vitamin A, vitamin D, vitamin E, vitamin C, folate, calcium, magnesium, fiber, and potassium
- Overconsumption of the following: Sodium, saturated fat, refined grains and added sugars
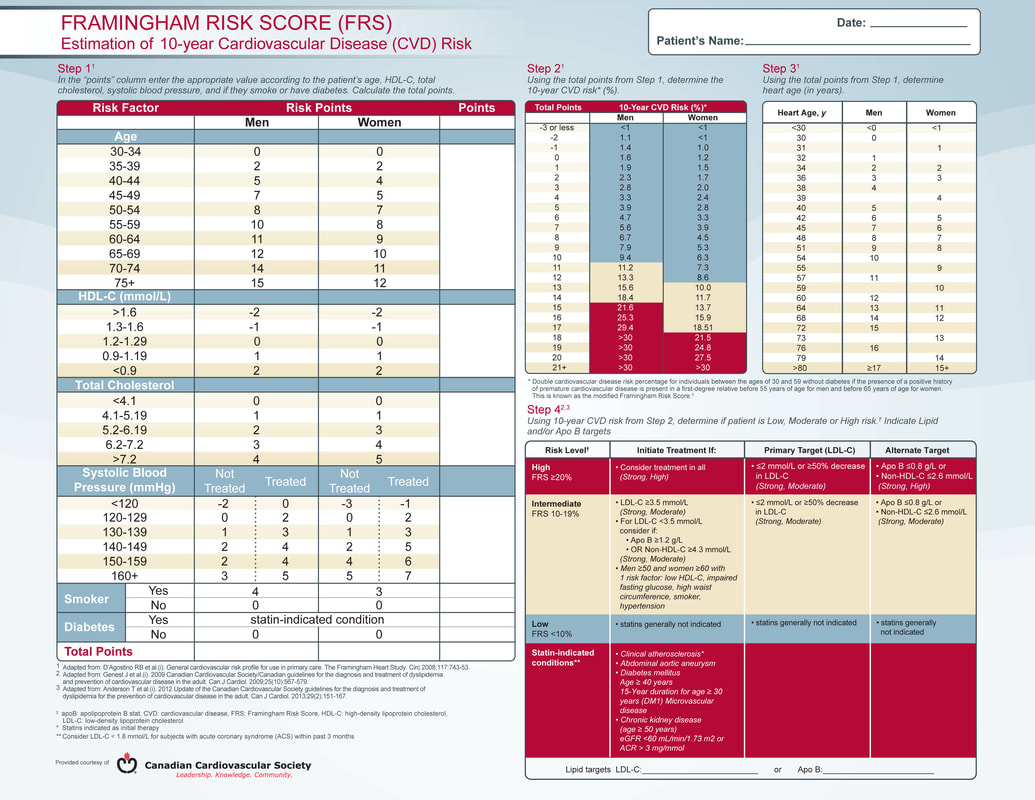
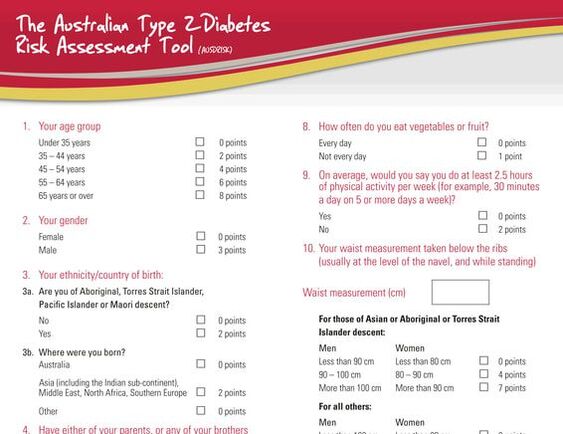
RISK FACTOR MEASUREMENT
- Environmental & Occupational factors
- Framingham risk assessment
- Diabetes risk assessment
- Fitness Assessment
- Mental and Emotional Health assessment
- Routine Laboratory tests. Conduct appropriate tests to screen, diagnose and monitor lifestyle-related diseases.
LIFESTYLE MEDICINE INTAKE FORM
Your objective is to know your patient's overall goals. Aside from the routine history taking and physical examination that you conduct during clinic visit there is more you need to know about your patient so you can help him/her further engage to a healthy behavior. Most doctors are using a very short intake form and often times neglecting initial assessment needed to see the root cause of the health problem.
TIPS:
- Never forget Medical and Social History
- Dietary and Physical Activity History
- Questions to be answered: By making a Lifestyle Medicine appointment, what do you hope to achieve? What are your intentions for this visit?
- Evaluate a patient's current health status in the context of their life journey
- Use effective health assessment tools for proper whole person lifestyle medicine diagnosis and treatment plan, not only physical conditions or "downstream" behaviors.
- Utilize a consistent lifestyle "vital signs" system
- Recognize the role of emotional health status of patients seeking medical care
TASK - Clinical Application |
STEP 1: Create your own Lifestyle Medicine Intake Form basing on the references and materials provided in this module. STEP 2: Ask at least 3 patients who have chronic disease to fill up your form (3 different cases). STEP 3: Examine the information you got from your patients. Analyze the correlation of those data with the established lifestyle risk factors you learned from the articles, and then create your Reflective journal. |