MODULE 3 - Lifestyle Medicine Clinical Processes (Part 1) |
|
Objectives:
|
INTERDISCIPLINARY PRACTICE
Lifestyle medicine health care providers are honed to develop the ability to practice as an interdisciplinary team of health care professionals. It is the best approach to establish a referral network for dietitians, exercise physiologists, culinary medicine specialists, lifestyle medicine coaches and other professionals. Network will definitely vary on the practice setting and the target population.
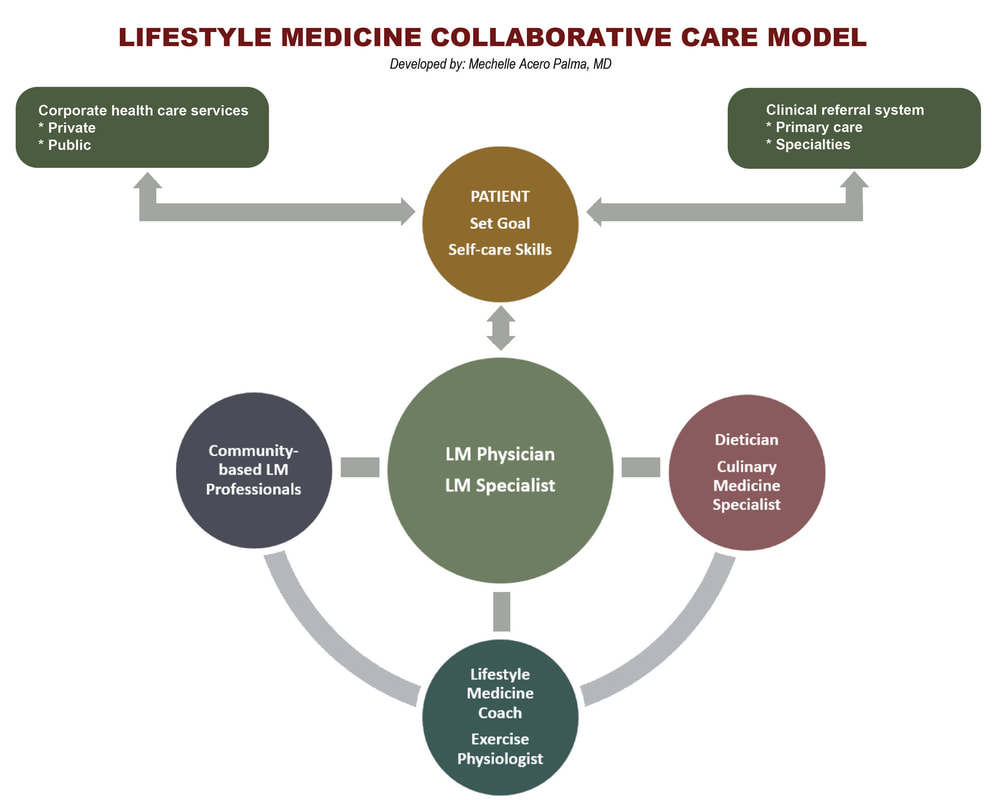
LIFESTYLE MEDICINE COLLABORATIVE CARE MODEL
Effective and efficient lifestyle medicine interdisciplinary practice can be implemented when the physician and the rest of the team are trained and equipped as educators, coaches, leaders and collaborators.
This model provides the support systems needed to achieve successful behavior change with lifestyle prescriptions and efficient delivery of value-based care.
Collaborative care improves patients outcome and is associated with higher levels of treatment compliance and supports self-efficacy and self-management.
This model provides the support systems needed to achieve successful behavior change with lifestyle prescriptions and efficient delivery of value-based care.
Collaborative care improves patients outcome and is associated with higher levels of treatment compliance and supports self-efficacy and self-management.
The Ornish Spectrum Program is one of the best example of lifestyle medicine collaborative care model.
- Informed and activated patient working with a team using planned care focusing on self management support
- Collaborative health system with organizational support, clinical information systems, delivery system design and decision support.
- Community resources for sustainable support system
A lifestyle medicine facility may compose of the following team roles:
- Medical director
- Registered nurse - biometrics assessment, continuity of care and follow-up of chronic condition
- Registered dietician - one on one or group nutrition counseling
- Culinary medicine specialist/Chef - experiential training in food selection and preparation
- Exercise physiologist - individual and group fitness supervision
- Lifestyle medicine coach - mechanism implementation, group facilitation and support
- Program director - oversees efficient and effective program implementation and delivery, monitoring & evaluation
- Group support specialist - facilitate social dynamic group growth
- Administrative assistant - scheduling, follow-ups, referrals, coordination of materials utilized in the programs
- Marketing director - communication with providers (primary care/specialties) and corporate resources
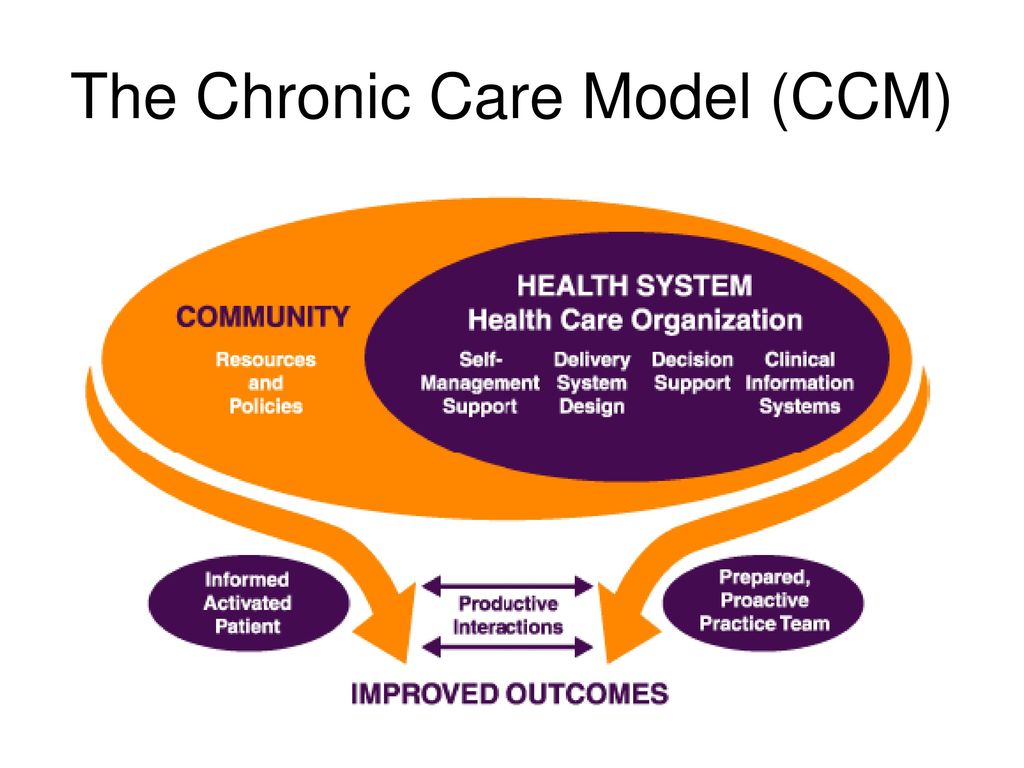
CHRONIC CARE MODEL
The primary purpose of chronic care model is to reduce fragmented care delivery while improving health outcomes at an acceptable cost to the healthcare system. The strategy was first introduced by MacColl Institute for Healthcare Innovation at Group Health Cooperative, commonly referred to as the Wagner chronic care model (WCCM) which is basically based on six key elements:
|
CHRONIC CARE MODEL IMPLEMENTATION GUIDELINES
Community Linkages. Linkages between your practice and community resources play important roles in managing your patients' chronic condition
Health Care Delivery System. Delivering the highest quality of health care is dependent of redesigning care in a fundamental way throughout the entire organization.
Self-Management Support. Effective self-management support can help patients and families cope with the challenges of living with and treating chronic illness. Patients and families become experts in the management of their chronic disease in partnership with their physician and care team. The patient-centered process can reduce complications and symptoms and improve patients' overall sense of health and well being.
Delivery System Design. Effective chronic illness management usually requires a continuous healing relationship and changes in the way offices provide care for patients, i.e., changes in your office systems and your way of doing business. Teamwork and continuous access are two important elements of effective chronic disease management.
Decision Support. Effective chronic illness management programs assure that physicians have access to evidence-based information necessary to care for patients to assist them in decision making. This might include evidence-based practice guidelines or protocols and other information sources that are readily available at the point of care.
Clinical Information Systems. Timely, useful information to guidelines and provide prompts and reminders about needed services (lab and other testing).
Community Linkages. Linkages between your practice and community resources play important roles in managing your patients' chronic condition
- Seek community-wide coordination between your office and community agencies in caring for patients.
- Partner with community organizations to develop formal supportive programs and policies across the entire system.
Health Care Delivery System. Delivering the highest quality of health care is dependent of redesigning care in a fundamental way throughout the entire organization.
- Support improvement from senior leadership down
- Promote strategies aimed at comprehensive systems change
- Encourage open, systematic handling of errors and quality problems
Self-Management Support. Effective self-management support can help patients and families cope with the challenges of living with and treating chronic illness. Patients and families become experts in the management of their chronic disease in partnership with their physician and care team. The patient-centered process can reduce complications and symptoms and improve patients' overall sense of health and well being.
- Emphasize patients' central role in managing their health care.
- Systematically assess patients' self-management needs and use peer support groups routinely.
- Train physicians and staff in behavior change techniques and encourage use of these skills as an integral part of routine care.
Delivery System Design. Effective chronic illness management usually requires a continuous healing relationship and changes in the way offices provide care for patients, i.e., changes in your office systems and your way of doing business. Teamwork and continuous access are two important elements of effective chronic disease management.
- Implement planned patient care with strategic visits and call reminders, online communications (E-visits), group visits, checking on patients between visits and identifying missed elements of care.
- Install an electronic health record with clinical decision support and a patient portal for their personal health record and for communication with the care team.
Decision Support. Effective chronic illness management programs assure that physicians have access to evidence-based information necessary to care for patients to assist them in decision making. This might include evidence-based practice guidelines or protocols and other information sources that are readily available at the point of care.
- Integrate evidence-based guidelines into care through reminders and other proven behavior change methods.
- Give patients guidelines with personalized targets for them to achieve and with recommendations about how to achieve the targets.
Clinical Information Systems. Timely, useful information to guidelines and provide prompts and reminders about needed services (lab and other testing).
- Tie patient registry and/or electronic health record information to guidelines and provide prompts and reminders about needed services (lab or other testing).
- Set up reminders for the care team about guideline adherence at the time of individual patient encounters.
- Give timely, specific performance feedback to each physician, by routinely reviewing reports. Correct any deficiencies as rapidly as possible.
- Establish treatment targets and goals collaboratively. Include self-management as well as clinical goals. Adjust individual treatment goals and targets frequently with input from patients.
shared medical appointment
Shared medical appointments (SMs) are clinic visits where a groups of patients are seen by two or more health care providers in a concurrent sessions. Studies show the benefits in various contexts to reduce healthcare cost, improve treatment plan adherence and improve clinical outcome. SMA is also commonly referred to as group visits which is a classic example of team approach for chronic disease management. It can be a supportive group setting of consenting patients with similar health concerns facilitated by 2-4 health professionals including a physician. There are numerous benefits of conducting SMA which gained popularity in US and Canada.
Benefits to Patients (Noffsinger 2019)
Benefits to Doctors (Noffsinger 2009)
Benefits to Clinics (Noffsinger 2009)
Operation of Group Visits
Benefits to Patients (Noffsinger 2019)
- Prompt access to care;
- Extra time with their own physician and more relaxed pace of care;
- Answers to questions they might not have thought to ask;
- Greater patient education and attention to psychosocial issued; Mind as well as body needs are met;
- Personalized care
- Appropriate privacy is maintained at all times - private time with the physician is available as needed;
- A means of reaching out to the underserved patients who might be falling through the cracks;
- Enhanced physician-patient relationships;
- High level of patient and provider satisfaction;
- Closer follow-up care;
- An additional health care choice;
- 'Drop in' convenience (in DIGMA or Drop in Group Medical Appointments)
Benefits to Doctors (Noffsinger 2009)
- Is an effective tool for working smarter, not harder;
- Is an important tool for better managing both physicians' practices and chronic illness
- Provide opportunity for physicians to do something different, interesting, and fun;
- Enhances quality, outcomes and the patient's health experience;
- Contains costs and increase the doctor's income
- Leverages existing resources to increase doctor productivity;
- Is a solution to access problems to doctor's practices and chronic illness treatment programs;
- Allow doctors to enjoy more time with patients, a more relaxed pace of care, and a temporary reprieve from ongoing clinic demands and distractions;
- Offer backlogged physicians the opportunity to provide closer follow-up care;
- Is a chance to get to know patients better
- Consistently high levels of patient and physician professional satisfaction;
- An opportunity to get off the fast-paced treadmill of individual office visits;
- Reduced patient phone call volume and complaints about access to care;
- Decreased need to work in or double-book patients;
- Documentation support is provided;
- Real help from the multidisciplinary team
- Additional collegial support from other patients'
- Reduced repetition of information;
- Increased opportunity from providing patient education and addressing motivational and psychosocial needs;
- A helpful tool for managing difficult, time consuming and psychologically needy patients.
Benefits to Clinics (Noffsinger 2009)
- Improved quality of care (max-packed visits, improved health maintenance, etc.)
- Improved access at both the individual physician and departmental level;
- Increased efficiency and the leveraging of existing resources;
- Dramatically increase physician productivity of 200-300% or more;
- Better management of back-logged practices;
- An important tool in chronic illness population management programs;
- High levels of patient and physician professional satisfaction;
- The competitive advantage of a new service and an additional healthcare choice;
- Improved focus for the clinic;
- Potential for increasing revenue and leveraging existing resources while reducing costs to the health system.
Operation of Group Visits
- Physicians manage, advise and treat each patient individually, but in front of others (except for brief private discussions and examinations)
- Avoids repetition
- Increases patient education
- Allows others who are present to listen, learn, ask questions, and actively participate
- Patients sign a confidentiality release in which they consent to having their medical information discussed in front of others and agree not to discuss the personal information of others once the group is over.
- Majority of patients are typically prescheduled
OFFICE SYSTEMS
Like in any medical practice it is important to develop and apply office systems and practices to support lifestyle medical care including decision support technology to implement office flow to effectively identify and address patient's needs. This will optimize time with patient for support, counseling, tracking lifestyle change progress, assess the need of intensive lifestyle interventions and for follow-up.
INFORMATION SYSTEMS
Depending on the set up of the lifestyle medicine center, the information system can be digital or paper based composing of patient registries for conditions and risk factors to support proactive care. Both system needs to send reminders with actionable feedback at appropriate point of care. Office systems should include:
MONITORING AND EVALUATION
Measure processes and outcomes to improve quality of lifestyle interventions in individuals and groups of patients to assure a team member conducts routine key processes. You have to work with a health care team to routinely plan, implement, and assess efficiency of program implementation for process and outcomes improvements.
INFORMATION SYSTEMS
Depending on the set up of the lifestyle medicine center, the information system can be digital or paper based composing of patient registries for conditions and risk factors to support proactive care. Both system needs to send reminders with actionable feedback at appropriate point of care. Office systems should include:
- Clinical decisions and care
- Tracking of lifestyle change progress
- Screening frequency
- Recording of test results
- Implementation of referral system and
- Recommended follow-ups
MONITORING AND EVALUATION
Measure processes and outcomes to improve quality of lifestyle interventions in individuals and groups of patients to assure a team member conducts routine key processes. You have to work with a health care team to routinely plan, implement, and assess efficiency of program implementation for process and outcomes improvements.
TASK - Application |
Basing on the description of lifestyle medicine collaborative care model, and the evidences you read in implementing shared medical appointments (SMAs), create your own proposed chronic care plan including the flow of referral for a specific lifestyle-related disease (e.g. diabetes, hypertension, heart disease, cancer, obesity, dyslipidemia, etc.). |