|
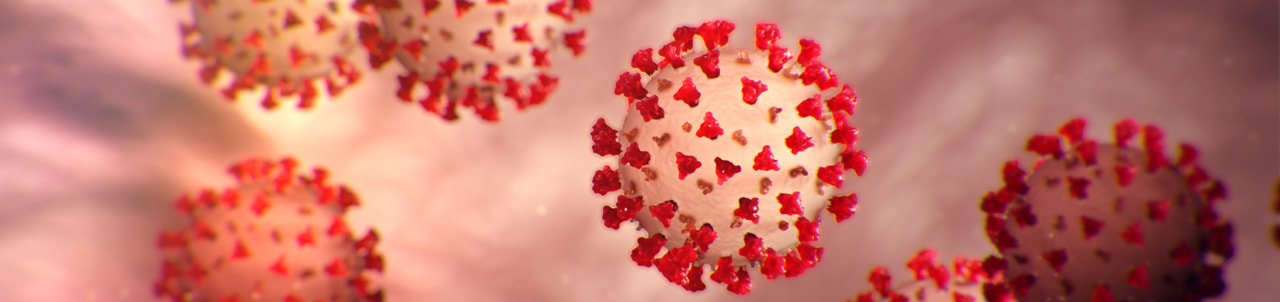
UPDATED MARCH 18, 2020 I MECHELLE ACERO-PALMA, MD The majority of the world's population is now getting acquainted with COVID-19 and its fatality to every affected person and the community at large. The health sector is exhausting all its capacity to provide care for infected people. Multiple collaborations of several government agencies are creating and implementing strategies to address every emerging concern. The media industry is giving its best effort to provide information and updates from authorities to the grassroots. But one potential preventive measure and strategy underemphasized by most media reports and campaigns include evidence-based LIFESTYLE INTERVENTION. A proven measure that anyone can implement to boost immune response may effectively address the need to decrease susceptibility and vulnerability to develop the critical condition due to COVID-19. The real frontliners are the people who are supposed to be educated of their responsibility of taking charge of their health and exhausting any possible resources and capacity to live healthfully and maintain an excellent immune function. There is no clear assurance that COVID-19 will be totally eradicated as it constantly mutates. Early studies are showing possibilities that it will be here to stay. Hence, the best mindset to develop is getting our body ready whenever we contract the virus at any given time. We will be discussing some salient points that each one should understand so we can have the advantage of preventing the disease from spreading and, most importantly, getting our cells ready to combat the viral invasion. WHAT IS NOVEL CORONAVIRUS? We should know the enemy. It is called Novel because it's a new Respiratory disease. We've seen and heard many names such as Coronavirus, COVID-19, SARS-CoV-2, and SARS. This is an RNA virus that can reproduce, and on its surface is a capsule with spikes forming a crown that's why it's called Coronavirus. In 2019 this Coronavirus created a disease outbreak in China, where it has gotten the name COVID-19. Then the World Health Organization created the official scientific name SARS-CoV-2 because this is the second generation daughter virus of SARS6. Scientists were given a heads up in 2003 to understand the nature of this family of Coronavirus. With the advent of genomics, they were able to understand how contagious the Coronavirus is. And sadly, due to mutations, it has allowed SARS-CoV-2 to become a thousand times more infective than SARS. Hence, a community quarantine was implemented in almost all countries affected to lessen the spread of infection. HOW CORONAVIRUS INFECT HUMAN CELL? It is essential to understand how the virus can get into the human cell and the consecutive effect of the virus in the body so we can have the opportunity to block it. An infected person can contaminate 2.6 other people through the droplets7. The nanoparticles of the virus form droplets and go to the hands and surfaces after an infected person coughs, sneezes, or even talk. Now the hands become a vector of disease as it carries the virus that can contaminate another person. That is already an advantage for us because we can always practice proper handwashing to effectively eliminate the virus.
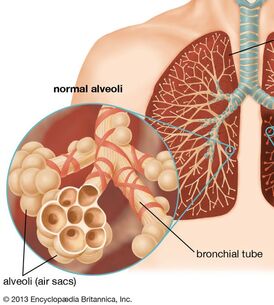
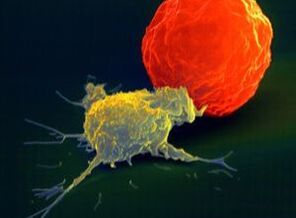
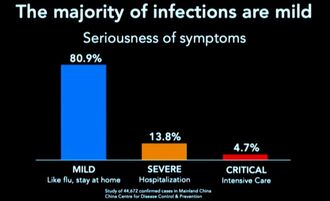
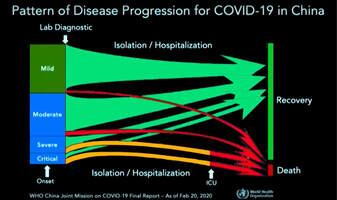
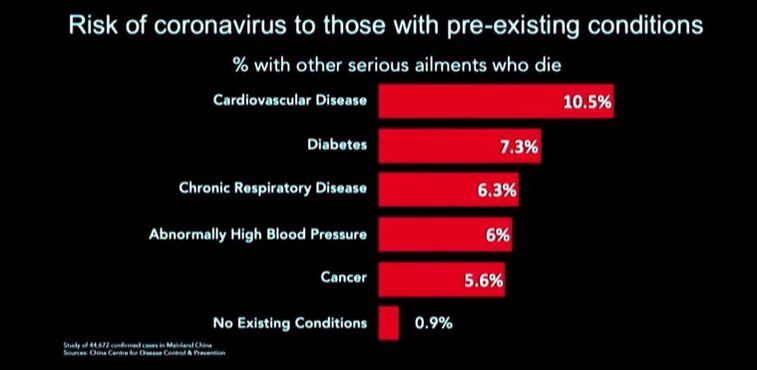
The virus takes advantage of the cell's machinery and uses it as the factory for viral replication. The virus is re-packaged, and then it sheds off the infected cell and propagate and eventually causes fibrosis in the lungs and leads to fatality9. HOW CAN WE STOP VIRAL PROPAGATION? In times of Pandemic where treatment is limited to alleviating symptoms, the only immediate solution is to have an effective immune response. It is also essential to understand that many people can get contaminated with any virus, but not all will get infected and end up with the disease. And that depends on multiple factors that include accessibility of virus to tissue, susceptibility to virus multiplication, the virulence of the virus, and the host immune response10. Our immune response depends on several biological and lifestyle factors that will be discussed in the next section. The immune system rests on two major pillars: the innate, general immune system and the adaptive, specialized immune system. Both systems work closely together and take on different tasks. The strength of the innate, general defense is to be able to take action very quickly. Because of this broad effect, it is only capable to a certain degree of stopping viruses from spreading in the body. Inflammatory cells move to the site of infection, and the complement system is activated, too, and helps to defend the body. This leads to an inflammatory reaction where blood circulation is increased and fever sets in. If the body’s first line of defense – the innate immune system – is unsuccessful in destroying the pathogens, the specific adaptive immune response sets in after about four to seven days. The adaptive immune system can remember the virus because it produces memory cells. This is also the reason why there are some illnesses you can only get once in your life because afterward, your body becomes “immune.”13. Take note of the two crucial immune cells that deal with viruses: The Natural killer cells (NK cells) and the Cytotoxic T-cell (T-killer cell). The NK cells are white blood cells (lymphocytes) that are aggressive first responders activated during a viral invasion. They specialize in identifying cells that are infected by a virus by looking for changes in cell surfaces. If natural killer cells find cells with a changed surface, they dissolve them using cell poisons, also called cytotoxins. They serve to contain viruses while the adaptive immune response generates antigen-specific Cytotoxic T cells that can clear the infection at a given period. It is essential to be familiar with the crucial key players in the immune response against viral infection. We need to know how to boost their function and avoid factors that may suppress their performance. The Natural killer cells are part of our Innate Immunity produced by the bone marrow and are found to be lodging in the lymph nodes, tonsils, and spleen. Whenever a virus comes in contact with human cells, the NK cells immediately take the first move. Unfortunately, the Coronavirus can stay in the body for more than thirty (30) days, and it can manage to find a way to evade the immune system and kill the Natural killer cells and the T-cell s in the body. As shown on data from China's experience, elderly patients who died of COVID-19 have low Natural killer cell and T-cell count7. However, it is well established that there is an age-associated decline of NK cell function responsible for many biological processes taking place during immune response8. Cigarette smoking also decreases the number and activity of NK cells in the lungs18. HOW TO RECOGNIZE AN INFECTION? Based on China's data, with over 44,000 cases, fever and dry cough are the hallmarks of the disease. This means that any person who develops fever and cough even without a test should suspect for infection and immediately proceed to self-quarantine to prevent potential contamination and infection spread. Signs and symptoms of COVID-19 also include body pains (myalgia/arthralgia), headache, difficulty of breathing, and diarrhea. Studies showed that 80.9% of infections are mild, 13.8% may go through severe infection, and 4.7% can develop critical condition7. Now we need to explore the known risks factors of advancing from mild to the critical stage of infection. RISK OF INFECTION & FATALITY AMONG INFECTED PERSON Any factors that disrupt Immune function makes a person at risk to contract an infection and eventually leads to fatal condition:
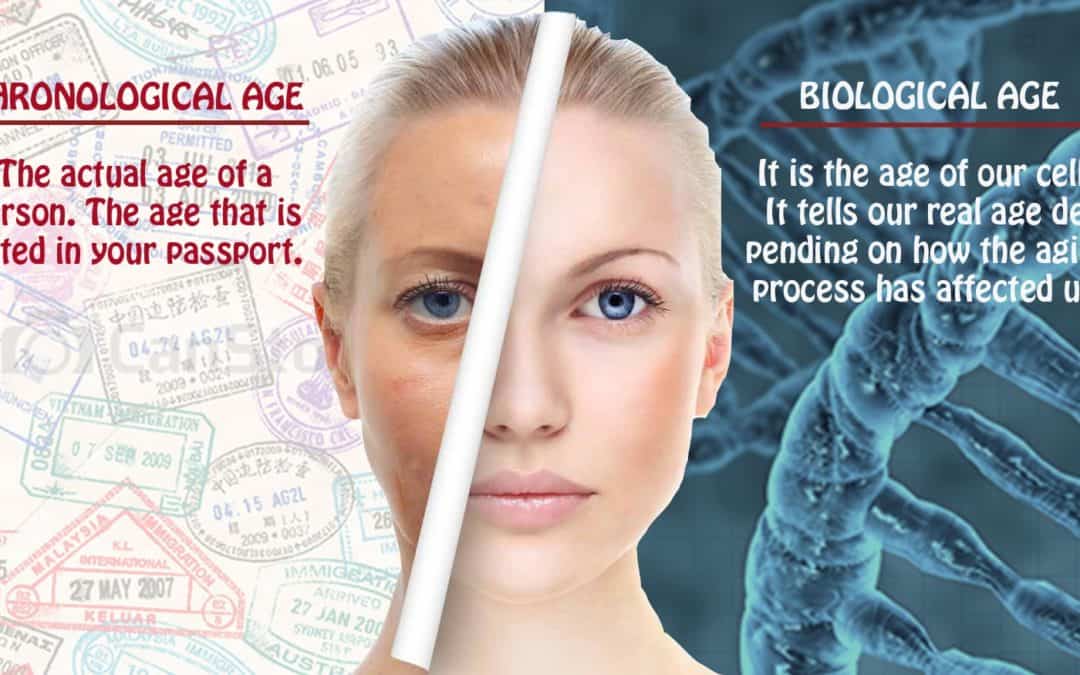
Aging and the immune System We all know the changes that occur as a person ages, and apparently, people age differently. Aging occurs at different levels of inquiry, biological, psychological, sociological, etc. All these levels address functioning, but from different viewpoints. This really means that the perceived age may vary from the actual chronological age, based on the usual presentation of individuals at a given calendar age. Performing as the first line of defense against COVID-19, natural killer (NK) cells as critical effector cells of the innate immune system is significantly impaired in elderly subjects. Such decreased NK cell activity has been shown to be associated with an increased incidence and severity of viral infection8. There is clear evidence that describes the state of profound age-associated changes in the immune system manifested by the overall decline of antigen-specific immunity. Lymphocytes are thought to have a finite replicative lifespan. Telomere length (tip of the chromosomes) may be the ultimate limit for the number of divisions that a human lymphocyte can undergo. Because telomeres are essential for maintaining chromosomal integrity, cells with critically shortened telomeres cease division (senescence) and are prone to die.
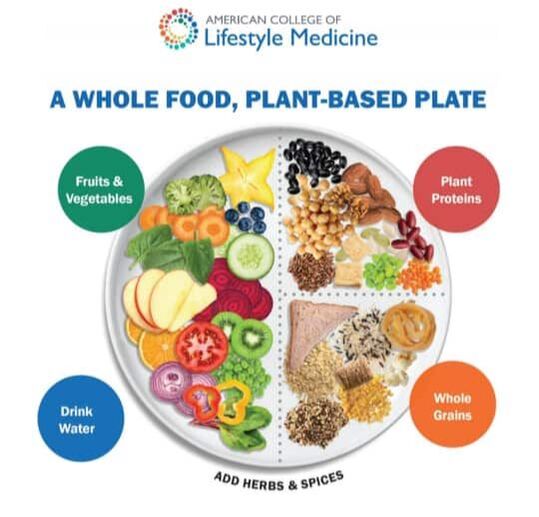
Aging is also associated with increased incidence of major diseases, including cancer, cardiovascular, neurodegenerative, metabolic, and autoimmune diseases which are comorbid conditions that may render an older adult vulnerable to COVID-1912. But as we look at the current statistics around the world, chronic diseases, which are thought to be a disease of old age, are now affecting people at an early age. Their telomeres are also shortening, which diminishes the integrity of the cell. Aging is determined by lifestyle, dietary habits, mental makeup, and even environmental factors and genetic factors. Faulty dietary habits, lifestyle, and stressful living may wrongly influence one's biological aging, which is the sole indicator of health and age-associated diseases15. So a person may only be 45 by chronological age may already be 65 by biological age. Impaired Immune Response for COVID-19 due to Noncommunicable diseases Comorbidity is the presence of one or more additional conditions co-occurring with a primary condition. The data shown by China established that a person with comorbidity has the highest risk of getting infected and developing a fatal condition and dying of COVID-19. Cardiovascular disease, diabetes, chronic respiratory disease, hypertension, and cancer documented pre-existing conditions of those who died during the disease outbreak7. Comorbidity is a known accurate predictor of impaired immunity than chronological age in adults. With increasing comorbidity in older adults, there is a proportional decrease in the immune response. The magnitude of impaired immunity depends on different specific illnesses and different levels of severity. It's not surprising to see healthy people aging 75 years old surviving COVID-19 while some 45 years old dying because of having underlying comorbidities20. The data clearly showed that the presence of Noncommunicable diseases (NCD) increases the risk of developing a fatal condition and eventually die when contracted with COVID-19. These chronic diseases are considered invisible epidemics that compose over 70% of the cause of mortality that is largely lifestyle-related and, therefore, preventable but under-appreciated23. Risk factors underlie the major NCDs are largely modifiable, including tobacco, harmful use of alcohol, unhealthy diet, insufficient physical activity, overweight/obesity, raised blood pressure, raised blood sugar, and raised cholesterol23. The long-standing NCD threat now also dictates the survival rate of persons infected with COVID-19. NCDs can be reduced using the existing evidence-based lifestyle intervention that offers highly proactive and cost-effective solutions. LIFESTYLE FACTORS THAT WILL BOOST ANTIVIRAL IMMUNE RESPONSE Adequate Sleep It is during sleep that repair and reversal of cell damage occur. Studies showed that alteration of immune function occurs even at a modest loss of sleep. The effect of early-night partial sleep deprivation is a reduction of natural immune responses on circulating numbers of white blood cells, natural killer cells, and cytotoxic T-cells. The killing activity of NK cells reduces by almost 30%. This implicates sleep in the modulation of immunity and demonstrates that even a modest disturbance of sleep reduces natural immune response, hence, subjecting the person to increased risk of viral infection1. In this generation, a huge percentage of people don’t meet the required number of sleep hours (7-8 hours) due to a wide variety of reasons. Exposing our eyes to Blue light suppresses the hormone MELATONIN, which is responsible for inducing sleep. The use of light-emitting diodes (LEDs) from electronic devices such as TVs, computers, smartphones, and tablets before bedtime may contribute to or exacerbate sleep problems. Exposure to blue-wavelength light, particularly these devices, may affect sleep by suppressing melatonin and causing neurophysiologic arousal17. Staying away from blue light spectrum exposure before the target time of sleep is necessary to achieve effective sleep. One proven way of improving sleep is to get good sunlight exposure in the morning. Daylight exposure could delay the sleep phase and correction of the circadian rhythm. Anxiety and insomnia could also be improved with daylight exposure with added activation of Vitamin D in the skin, which is also necessary to boost immune functionn16. The timing and amount of food intake at night were also found to affect the quality of sleep. Researchers at Brazil's Universidade Federal de São Paulo studied the relationship between food intake and sleep patterns in a group of healthy young adult men and women. They found that eating more heavily at night was associated with deterioration to several measurements of sleep quality. They also found that women were more vulnerable to the negative effects of nighttime eating on sleep. Having a light meal during dinner will greatly help attain good quality of sleep. Adequate Physical Activity Research showed that moderate physical activity might improve the function of immune cells. Moderate physical activity is specific for every person. You can tell when you are doing the moderate physical activity if you can no longer sing while doing your exercise. While regular exercise improves the natural immune response, following strenuous and exhaustive exercise will decrease the number of NK cells, and their activity is depressed for several days. On the other hand, Sedentary behavior, characterized by a sitting or reclining posture and low-energy expenditure, has been recognized as an independent health risk factor. Evidence shows that being sedentary is associated with an elevated risk of insomnia and sleep disturbance and ultimately affects the immune response2. Regular physical activity should be matched with the age and the capacity of an individual to move. There are a variety of ways to increase physical activity, even during periods of self-quarantine or isolation. Seated exercises and stationary walking are some very common examples of activities that anyone can do with the help of available online instructional videos. Exercise causes the heart to pump blood into the circulation more efficiently, resulting in increased oxygen delivery and increased perfusion of tissues and organs with blood components, including the immune cells. Right Food Combination for Nutritional Immunology A well-functioning immune system is critical for survival. It should be constantly alert in monitoring for signs of invasion by distinguishing self from non-self and discriminating against harmful molecules like pathogens. A well-balanced whole food plant-based diet (WFPB) enhances immune function in contrast with meat and refined carbohydrates. It is imperative to have a better understanding of the role of diet and nutrients in immune function. Adequate and appropriate nutrition is required for optimal function of "activated" immune cells, allowing them to initiate effective responses against pathogens, increasing the basal energy expenditure during infection periods. High resveratrol intake on a regular basis was also noted to have immunomodulatory properties. These can be found in plant-based sources such as peanuts, grapes, soy, and berries. Avoiding sugary food and beverage is also extremely important to prevent suppression of immune response. Alcohol and smoking also increase one's risk for viral infection2. Avoiding processed food, meat products, and refined carbohydrates are known causes of gut microbiome disruption or dysbiosis that will alter immune homeostasis. Remember that our gut wall houses 70% of the cells that make up our immune system. So the gastrointestinal system plays a central role in our immune system homeostasis. It is the main route of contact with the external environment and can be overloaded every day with pathogens or toxic substances3. Consuming naturally prepared whole-food plant-based meals will significantly change the composition of the gut microbiome in favor of a positive immune response.
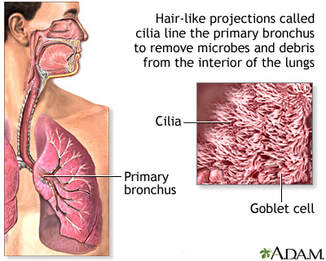
The Power of Positive Mental Attitude Studies have shown that stress and depression reduce NK cells and T-killer cells' ability to respond to viral infection. However, positive thinking and problem-solving coping skills can improve NK cells activity even in stressed individuals. Regular exercise is thought to be associated with stress reduction and better mood, which may partly mediate associations between depression, stress, and health outcomes and its potential role of the inflammatory response as a central mechanism. Psychosocial factors, such as chronic mental stress and mood, are significant predictors of longevity and well-being. In particular, depression is independently associated with cardiovascular disease all-cause mortality, diabetes, obesity and is often comorbid with chronic diseases that can worsen their associated health outcomes4. While people face fear, stress, and uncertain lifestyle adjustments due to the current crisis, We are seemingly left with only one choice: to protect ourselves through boosting immune response. Think about Neuroplasticity, the ability of our brain to recognize itself in response to situations and changes in the environment. We can always choose to create a new Neurological pathway leading to a Healthy Lifestyle instead. Quit Cigarette Smoking and Avoid Alcohol Aside from compromising the respiratory cilia, smoking impacts both innate and adaptive immunity and plays dual roles in regulating immunity by either exacerbation of pathogenic immune responses or attenuation of defensive immunity. Smoking also plays a complex role in numerous diseases, including cardiovascular, respiratory, and autoimmune diseases, allergies, and cancers21 These are known comorbidities that increase the risk of a person contracting a viral infection and eventually developing a fatal condition. There is no other way to go but to deliberately quit smoking with the help of your health care provider if needed so. Alcohol disrupts immune pathways in complex ways. These disruptions can impair the body’s ability to defend against infection, contribute to alcohol’s combined effects on innate and adaptive immunity, significantly weakening host defenses, and predisposing chronic drinkers to a wide range of health problems, including infections and systemic inflammation. Alcohol also interferes with the developing immune system in the fetus, and this exposure increases a newborn’s risk of infection and disease deleterious effects on immune development last into adulthood. Alcohol also alters the composition of the gut microbiome, an extensive community of beneficial microorganisms in the intestine that aid in normal gut function. These organisms affect the maturation and function of the immune system. Alcohol disrupts communication between these organisms and the immune cells with essential implications beyond the intestinal immune system. Alcohol disrupts ciliary function in the upper airways, impairs the function of immune cells, and weakens the barrier function of the epithelia in the lower airways. Studies showed that alcohol-provoked lung damage often goes undetected until a second insult, such as a respiratory infection, and leads to more severe lung diseases than those seen in nondrinkers22. PROACTIVE AND PREVENTIVE APPROACH Just like the way we think about any other mainstay and seasonal viruses we co-exist with, ROBUST IMMUNE RESPONSE is always associated with self-limited clinical recovery. But due to our modern LIFESTYLE, we are exposing ourselves to many various factors that don't favor boosting our immune system at all. Just when we thought that it's mostly Noncommunicable diseases that will be impacted by LIFESTYLE MEDICINE, experts are now starting to realize and appreciate more than ever that our NATURAL IMMUNE RESPONSE which largely depends on HEALTHY BEHAVIORS is the first line of intervention in the level of Prevention, Management and Recovery from Communicable diseases. This is specifically true for a new type of viral disease where ample time is needed to create immunization or a pill that will only mimic the weapon naturally used by our immune system. Indeed, the hardest battle is fighting with the unseen, not just the COVID-19 but mostly the battle between so many choices and habits that became part of our modern lifestyle. The good news is that we can always initiate a behavior change and reorganize to finally lead us to live an OPTIMAL LIFESTYLE that will not only shield us from infectious disease but mostly from a non-communicable disease that is taking over a thousand lives of Filipinos every single day. Learn and Share References:
1. Irwin M, McClintick J, Costlow C, Fortner M, White J, Gillin JC. Partial night sleep deprivation reduces natural killer and cellular immune responses in humans. FASEB J. 1996 Apr;10(5):643-53. PubMed PMID: 8621064. 2. BioMed Centra. "ALcohol impairs the body's ability to fight off viral infection, study finds." ScienceDaily, 2 October 2011. www.sciencedaily.com/releases/2011/09/110929235156.htm 3. Yang Y, Shin JC, Li D, An R. Sedentary Behavior and Sleep Problems: a Systematic Review and Meta-Analysis. Int J Behav Med. 2017 Aug;24(4):481-492. doi: 10.1007/s12529-016-9609-0. Review. PubMed PMID: 27830446. 4. Vighi, G., Marcucci, F., Sensi, L., Di Cara, G., & Frati, F. (2008). Allergy and the gastrointestinal system. Clinical and experimental immunology, 153 Suppl 1(Suppl 1), 3–6. https://doi.org/10.1111/j.1365-2249.2008.03713.x Hamer M, 5. Endrighi R, Poole L. Physical activity, stress reduction, and mood: insight into immunological mechanisms. Methods Mol Biol. 2012;934:89-102. doi:10.1007/978-1-62703-071-7_5. PubMed PMID: 22933142. 6. Naming Corona Virus Disease (COVID-19) and the virus that cause it. World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. 7. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report. 8. Hazeldine, Jon, and Janet M Lord. “The impact of ageing on natural killer cell function and potential consequences for health in older adults.” Ageing research reviews vol. 12,4 (2013): 1069-78. doi:10.1016/j.arr.2013.04.003 9. The American Journal of Pathology. "Pathology and Pathogenesis of Severe Acute Respiratory Syndrome." https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1829448. 10. Samuel Baron, Michael Fons, and Thomas Albrecht. Medical Microbiology. "Viral Pathogenesis". Chapter 45. https://www.ncbi.nlm.nih.gov/books/NBK8149. 11. Jazwinski SM, Kim S. Examination of the Dimensions of Biological Age. Front Genet. 2019;10:263. Published 2019 Mar 26. doi:10.3389/fgene.2019.00263. 12. Gian Andrea Rollandi 1, Aldo Chiesa 1, Nicoletta Sacchi 1, Mauro Castagnetta 1, Matteo Puntoni 1, Adriana Amaro 2, Barbara Banelli 2, Ulrich Pfeffer 2.OBM Geriatrics. Biological Age versus Chronological Age in the Prevention of Age Associated Diseases. 13. Aoshi T1, Koyama S, Kobiyama K, Akira S, Ishii KJ.Innate and Adaptive Immune Response to Viral Infection and Vaccination. Curr Opin Virol. 2011 Oct;1(4):226-32. PubMed PMID: 22440781. 14. Weng NP. Aging of the immune system: how much can the adaptive immune system adapt?. Immunity. 2006;24(5):495–499. doi:10.1016/j.immuni.2006.05.001. 15. Samarakoon SM, Chandola HM, Ravishankar B. Effect of dietary, social, and lifestyle determinants of accelerated aging and its common clinical presentation: A survey study. Ayu. 2011;32(3):315–321. doi:10.4103/0974-8520.93906. 16. Karami Z, Golmohammadi R, Heidaripahlavian A, Poorolajal J, Heidarimoghadam R. Effect of Daylight on Melatonin and Subjective General Health Factors in Elderly People. Iran J Public Health. 2016;45(5):636–643. 17. Tosini, Gianluca et al. “Effects of blue light on the circadian system and eye physiology.” Molecular vision vol. 22 61-72. 24 Jan. 2016. 18. Hervier B, Russick J, Cremer I, Vieillard V. NK Cells in the Human Lungs. Front Immunol. 2019;10:1263. Published 2019 Jun 4. doi:10.3389/fimmu.2019.01263. 19. Shammas MA. Telomeres, lifestyle, cancer, and aging. Curr Opin Clin Nutr Metab Care. 2011;14(1):28–34. doi:10.1097/MCO.0b013e32834121b1. 20. Castle SC, Uyemura K, Rafi A, Akande O, Makinodan T. Comorbidity is better predictor of impaired immunity than chronological age in older adults. J Am Geriatr Soc. 2005 Sep;53(9):1565-9. PMID:16137288 21. Qiu F, Liang CL, Liu H, et al. Impacts of cigarette smoking on immune responsiveness: Up and down or upside down?. Oncotarget. 2017;8(1):268–284. doi:10.18632/oncotarget. 13613. 22. Sarkar, Dipak et al. “Alcohol and the Immune System.” Alcohol Research : Current Reviews vol. 37,2 (2015): 153–155. 23. World health Organization, 2014. Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland: World health Organization.
2 Comments
5/19/2020 07:49:25 pm
Can you give us the lectures and videos presentation in my email.
Reply
4/21/2022 03:39:38 pm
Coronavirus is a significant issue right now in the world, and this blog is very informative on how to detect if you are affected by it. Can you tell me about some measures people can take to prevent the coronavirus?
Reply
Leave a Reply. |
AuthorMechelle Acero Palma, MD Archives
August 2021
Categories |
|
Working Hours
Monday to Friday: 8:00am to 5:00pm Online course: 24/7 |
The Philippine College of Lifestyle Medicine is an Affiliate Specialty Society of the Philippine Medical Association under the division of the Philippine Academy of Family Physicians

 RSS Feed
RSS Feed



